Alzheimer's disease (AD) is the most common cause of dementia, impacting roughly 44 million people worldwide.
In some nations, those numbers could triple in the next fifty years, and scientists are desperately trying to find ways to protect our aging populations.
Now, a novel method for treatment has been shown to successfully immunize mice against animal models of AD.
We still don't know if the approach can be used to vaccinate humans against the disease, but the results look promising compared to other attempts. The authors are now calling for commercial partners to help them take the research further.
"While the science is currently still at an early stage, if these results were to be replicated in human clinical trials, then it could be transformative," says drug researcher Mark Carr from the University of Leicester in the UK.
"It opens up the possibility to not only treat Alzheimer's once symptoms are detected, but also to potentially vaccinate against the disease before symptoms appear."
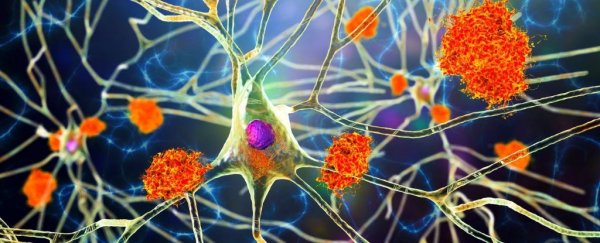
One of the hallmarks of Alzheimer's disease are the plaques of amyloid beta proteins (Aβ) that can be found in the brains of roughly two-thirds of clinically diagnosed patients post-mortem.
Amyloid beta proteins on their own aren't necessarily bad for cognition – their presence may actually be important for brain health – but when some truncated forms appear and clump together, research suggests they can grow toxic, leading to neurodegeneration.
Other AD treatments that target amyloid beta proteins indiscriminately have been shown to have adverse impacts, but this new immunization approach only targets the toxic truncated proteins.
Researchers had identified a family of antibodies called TAP01 in mice that could neutralize the truncated proteins while leaving healthy full-length ones alone. These antibodies could therefore be a useful way to stop the truncated proteins from binding with each other.
To make sure these antibodies work for humans, too, the authors created a version of the antibody for our own species, called TAP01_04.
Using X-ray crystallography to peer closer at the action of the TAP01_04 antibody in the brain of a transgenic 'humanized' mouse, the team noticed it was binding to a region of the truncated proteins that looked sort of like a hairpin.
The result not only reduced plaque load in the mouse brain, it also rescued glucose metabolism, memory deficits, and neuron loss.
By engineering a similar hairpin-shaped protein, researchers then created a more direct 'vaccine', called TAPAS. By mimicking the truncated proteins, this vaccine triggered the mouse immune system to produce TAP01 type antibodies of its own accord.
When this vaccine was given to two mouse models of preclinical AD, it showed similar results to the antibodies on their own.
That's really exciting news, but while amyloid beta plaques are associated with many forms of Alzheimer's, this vaccine might not be able to prevent all forms of the disease.
Emerging evidence suggests AD is more than just one thing and may include multiple subtypes. In about a third of patients with clinical diagnoses, for instance, amyloid beta plaques are missing postmortem, which means a vaccine against their forming may not prevent brain degeneration.
Nevertheless, if this potential new vaccine can make it through human clinical trials, it might just bolster the brain health of millions. Let's hope the researchers find a commercial partner to team up with soon.
"The results so far are very exciting and testament to the scientific expertise of the team," says biochemist Preeti Bakrania from the medical research charity LifeArc.
"If the treatment does prove successful, it could transform the lives of many patients."
The study was published in Molecular Psychiatry.