Fasting can slow the development of one of the most common forms of childhood leukaemia, new research has found.
Based on tests in mice, going without food on a regular schedule was enough to halt the progress of two types of acute lymphoblastic leukaemia (ALL), and there's hope that the findings could be used to develop treatments for cancer in humans, too.
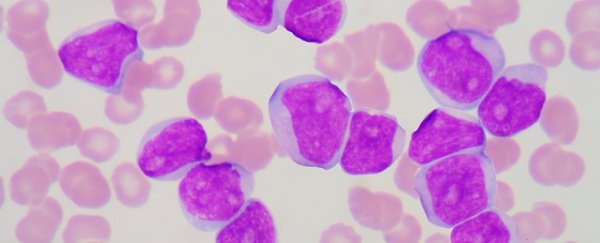
ALL is caused by the body overproducing immature white blood cells called lymphoblasts that gradually replace healthy ones – and while the cancer does occur in adults, it most commonly occurs in children.
But when mice with ALL were restricted in their eating patterns, researchers from the University of Texas Southwestern Medical Centre noticed a significant drop-off in the disease's effects.
"We found that in models of ALL, a regimen consisting of six cycles of one day of fasting followed by one day of feeding completely inhibited cancer development," says lead researcher Chengcheng Zhang.
"Mice in the ALL model group that ate normally died within 59 days, while 75 percent of the fasted mice survived more than 120 days without signs of leukaemia."
To test how fasting could be used to stop the disease, the researchers used fluorescent, coloured proteins to keep track of the cancer cells.
After seven weeks, virtually no cancerous cells were detected in the fasting mice, while an average of 68 percent of cells were found to be cancerous in the mice that hadn't been fasting.
Part of the treatment's success seems to be related to the hunger-inhibiting hormone leptin, which is created by fat tissue.
Previous research has shown that fasting can reduce leptin levels, and ALL patients often show weakened leptin receptor activity, so the researchers paid close attention to both factors during their study.
They found that intermittent fasting in mice increased leptin receptor activity, and they think this fact is significant in the success of their treatment.
"We found that fasting decreased the levels of leptin circulating in the bloodstream as well as decreased the leptin levels in the bone marrow," explains Zhang. "These effects became more pronounced with repeated cycles of fasting."
"After fasting, the rate at which the leptin levels recovered seemed to correspond to the rate at which the cancerous ALL cells were cleared from the blood," he adds.
While fasting was capable of stopping the development of ALL, the technique wasn't as effective against another type of blood cancer that's more common in adults, called acute myeloid leukaemia (AML).
In tests with a mouse model of AML, the activity of leptin receptors was unaffected by fasting, which could explain why restricted eating doesn't seem to help against this different form of leukaemia.
Of course, these tests have so far only been run on mice, so there's no guarantee that the same results would be seen in people.
But if scientists are able to develop a similar treatment for humans with ALL, there's one big advantage to this approach – deliberately skipping meals doesn't involve taking any drugs, so clinical trials can start sooner without any extensive testing of pharmaceuticals.
The researchers are now keen to test their findings further, with a view to ultimately figuring out how to simulate fasting mechanisms in the body, so that patients with the disease don't have to give up food to get better.
"It will be important to determine whether ALL cells can become resistant to the effects of fasting," says Zhang.
"It also will be interesting to investigate whether we can find alternative ways that mimic fasting to block ALL development."
The research has been published in Nature Medicine.