Placebos offer the tempting possibility of pain relief without drugs or surgery, largely relying instead on expectations that pain will go away.
As intangible and elusive as that sounds, the placebo effect is a very real thing, which scientists have now traced to specific neural circuits in the brain in a recent experiment based on mice.
What's more, in the process the team of researchers led by Chong Chen, an anesthesiologist at the University of North Carolina (UNC) Chapel Hill, also discovered that a part of the brainstem not previously known to be involved in pain processing actually is.
Scientists have been hunting for the biological basis of the placebo effect in the brain for years – a difficult thing to do when a person's response to a placebo is also wrapped up in psychology and likely influenced by past experiences that may condition them to think a certain way.
Expectations of whether or not a treatment or surgery will work and relieve pain also play into the placebo effect, over which the authority of doctors holds a lot of sway.
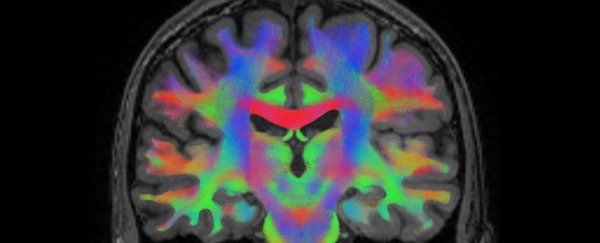
Brain imaging studies have revealed certain brain features thought to make people more susceptible to the placebo effect, including differences in the connectivity between the anterior cingulate cortex, the prefrontal region in front of it, and the brainstem below.
These regional changes, identifiable on brain scans, could be useful in predicting who might respond strongly to a placebo and how that may affect clinical trials. But to understand how the placebo effect arises and which brain cells are involved, we need to dig a little deeper.
Chen and colleagues probed neural circuits involved in pain relief in mice that had been conditioned to expect one side of a two-part chamber to be comfortably cooler than the other half, which was heated to a painful 48 °C (118.4 °F).
Though their effects on physiology can be variable and inconsistent, placebo treatments can demonstrably reduce patient discomfort or pain, even when they understand it's a sham.
This has given rise to the controversial idea that placebos could be given openly to patients as pain relief, to get around the ethical quandaries of deceiving people while still evoking an analgesic effect for the millions of people worldwide who endure chronic pain.
But the pain-relieving effect of placebos emerges from simply engaging in the ritual of medicine, regardless of whether the pill or potion is real or fake. This complicates clinical trials, making it harder for researchers to determine whether a new medication is effective in alleviating pain.
So it's little wonder researchers want to better understand the mechanisms underpinning the placebo effect and pain, beyond a surface-level understanding of the general brain regions involved.
In their animal experiments, Chen and colleagues showed that following a few days of conditioning, mice spent more time on what had been the cooler floor even though it was now also heated to 48 °C.
The conditioned animals also displayed fewer pain-relief behaviors, such as rearing up on their hind legs and licking their feet, suggesting they were able to tolerate the higher temperature because a pain-relieving placebo effect had kicked in.
To see which neural circuits were most active during the temperature tests, the researchers fitted the mice with miniature, head-mounted microscopes and measured the activity of neurons in the rostral anterior cingulate cortex (rACC), a region implicated by previous brain imaging studies.
This real-time imaging revealed networks connecting the rACC to the pontine nuclei – a part of the pons region of the brainstem understood to be involved in motor function – which became active when the placebo effect kicked in.
When the researchers knocked out this newfound pathway, the mice could no longer tolerate the painful hot floor, and when the team artificially activated these circuits, it stimulated a placebo effect in animals not conditioned to expect pain relief from the cooler floor first.
With further brain tissue staining, Chen and colleagues discovered that a "remarkably large proportion" of neurons in the pontine nuclei are studded with opioid receptors that control pain.
This suggests a new role for pontine nuclei in pain tolerance, which could be stimulated or targeted with drugs, electrodes, or therapies to treat pain.
But first, we'll have to see how the findings of these animal experiments translate to humans, whose pain experiences are far more complex.
The study has been published in Nature.