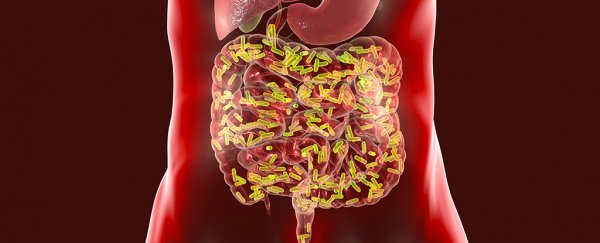
One thing we're not short on is research linking microbes living in our guts with the health of our brain and nervous system. Unfortunately, most studies are either circumstantial, or largely rely on animal models.
Now we have solid evidence in human volunteers that incidences of a rare neurovascular disease called cavernous angioma (CA) can be triggered by a particular mix of bacteria in our digestive tract.
None of this is to say animal studies don't have their place. In fact, the research team behind the finding were inspired by investigations on mice that hinted at just such a connection.
"The implications of that were very big," says University of Chicago neurologist and senior author Issan Awad, who was also on the team behind the original finding in rodents.
"But we didn't know if this concept of a unique microbiome that favours the development of lesions would be true in human beings."
Cavernous angiomas are lesions made up of unusually expansive blood vessels in the brain and spinal cord. Thankfully, it's not exactly a common disease, occurring in just 0.2 percent of the population.
The disease's impact depends largely on where these abnormal vessels develop. In some areas of the nervous system they can produce seizures, which often steadily worsen over time. In others it can lead to weakness in the limbs, problems with vision, or failing memory.
While it can pop up sporadically in individuals who have no history of the disease in their family, there is also a familial form of CA that's been associated with a small number of genes.
Of course, diseases are often rather complicated things, with numerous factors contributing to the development of symptoms.
To investigate the potential role bacteria are presumed to also play in the condition, the researchers collected faecal samples from more than 100 individuals who had a current diagnosis of either familial or sporadic forms of CA.
Similar samples were also collected from 250 volunteers who had no diagnosis for comparison.
A genetic analysis on both sets of specimens confirmed a clear relationship between the neurovascular condition and a predominance of gram-negative type bacteria.
"The CA patients from all the different collection sites had the same distinctive microbiome, regardless of whether they had inherited the mutation or had a sporadic lesion, and regardless of the number of lesions they had," says Awad.
In fact, the relative abundance of just three species could be used to reliably sort the people with CA from those without.
Those with greater amounts of a gram negative species called Odoribacter splanchnicus, and lower numbers of gram positives Faecalibacterium prausnitzii and Bifidobacterium adolescentis, were far more likely to have the condition.
Using machine learning to find patterns among the multitude of chemicals in blood samples, the team also found signs that key inflammatory receptors were being ramped up in CA patients.
Combined with the earlier studies, it's a strong bet that having more of some types of bacteria in the gut provokes an unusually high inflammatory response in the body that raises the risk of blood vessels in the brain developing abnormalities.
Knowing the chain of events that cause this condition is a huge step towards treating it. Unfortunately, that might not be as straight-forward as killing off offending species, and risking further problems by upsetting the balance of the microflora in the gut.
"This is more complicated than it appears," Awad acknowledges.
As we learn more about the nature of our body's microbial 'organs', no doubt we'll find better ways to tinker with its makeup, too.
This research was published in Nature Communications.