Blood vessels damaged by cardiovascular disease can become a serious problem if they're not repaired in time. To do that, you have two options: replace it with a vessel taken from another part of your body, or make a new one from scratch.
Option A has its limits. And the kinds of synthetic vessels we currently use for option B aren't risk-free. So researchers are exploring option C - get a dead body to make one for you.
The US-based biotech company Humacyte has made headway on a radical new method for building replacement blood vessels using tissues from recently deceased donors.
The results from two recent phase II clinical trials involving patients with end-stage kidney failure have shown their lab-grown vessels work just as predicted.
Rather than swapping a damaged vessel for a spare part taken from a cadaver and risking rejection, the company have developed a procedure that puts donated cells to work constructing a frame of proteins for the patient's own cells to grow on.
This approach promises some big advantages over current procedures.
If a blood vessel no longer functions as necessary, surgeons will usually dig out a replacement from another part of your body.
Hopefully they'll find one of suitable size and shape that isn't performing an essential role, but it's not an easy process. Even if the doctors happen to find such a replacement, there's a risk the graft simply won't take.
Meanwhile, a synthetic graft lets medical specialists to tailor the replacement to match the damaged part. Tubes constructed from various polymers might do the trick for some larger vessels, but when it comes to smaller pipes, healing becomes a problem.
A middle-of-the-road approach is to produce a frame for a blood vessel and populate it with the patient's own tissue. This might be a synthetic lattice of some sort, or a matrix of proteins from a donor's vessels with its own cells stripped away.
Even here, a major hurdle is encouraging the host's cells to quickly move into their new home. 'If you build it they will come' isn't always true when it comes to developing the infrastructure for tissue growth.
"Identifying when and what types of host cells participate in the repopulation and remodelling of implanted vascular material becomes critical for understanding their long-term success or failure in patients," the researchers state in their report.
Researchers at Humacyte are learning to manage this process by taking appropriate muscle and epithelial tissues from a cadaver and manipulating them into growing over a biodegradable mesh.
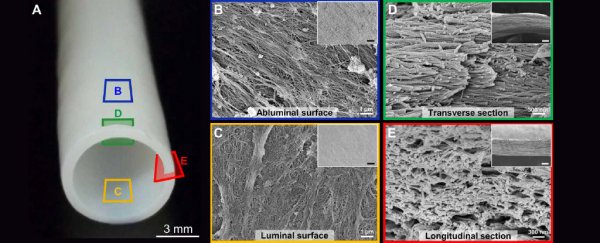
After eight weeks developing in a bioreactor, the donor's cells are stripped away. All that's left in the end is a stiff web of proteins they call a human acellular vessel, or HAV, which is capable of transporting blood on its own.
Without the donor's cells attracting the immune system's attention, there's nothing for the host's body to reject. The protein tubes are also far easier to produce and store in sufficient quantities.
"The removal of the cells is important so that the vessels can be manufactured in large batches and stored on the shelf in operating rooms for implantation into any patient," Humacyte's COO Heather Prichard told D-Brief Discovery blog writer, Roni Dengler.
Unlike other scaffolds, HAVs aren't subject to the same preservation or cell-stripping procedures that are thought to interfere with the uptake of host blood vessel cells.
To test the newly grown structures, the team actually grafted HAVs into the upper arms of 60 volunteers in the US and Poland who were suffering renal failure.
Ultrasounds conducted on the vessels up to a year after implantation showed an insignificant drop in blood flow, suggesting they were doing their jobs as hoped.
A total of 16 patients have had segments of HAVs removed for various reasons over the past few years, giving researchers an opportunity to take a closer look at how the host's cells settled into the grafts.
As hoped, the cadaver-produced matrix of proteins had grown layers of appropriate tissue resembling those of the patient's own blood vessels. The HAVs even showed clear signs of repair around sites where cannulation needles had punctured the vessel.
Heart disease remains a leading cause of death across much of the post-industrial world.
Of course changing our lifestyle is one way to avoid an early grave. But improving treatments with ready access to safe and reliable replacement vessels will surely be a life-saver for those who need it.
This research was published in Science Translational Medicine.