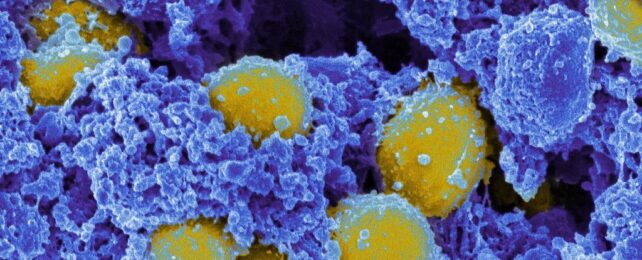
Golden staph are ubiquitous bacteria, living harmlessly on the skin or inside the nose of nearly one in three people worldwide.
Yet they are duplicitous, too. In some situations, golden staph (Staphylococcus aureus) can become monsters, causing dangerous infections in the skin, blood, bones, or elsewhere. Some strains are also drug-resistant 'superbugs,' armed with features that protect them from even our best antibiotics.
In a new study, however, researchers reveal valuable details about how these double-crossing bacteria hide inside human cells, a trick that helps them evade the defenses of our immune systems.
By shedding light on secrets like this, we may eventually find more effective ways to defang golden staph, offering humans a much-needed boost in our ongoing battle against superbugs.
S. aureus is a pathobiont, or a typically benign member of the microbiome that can run amok when given a chance. That may happen if the bacterium gets past its host's skin, perhaps enabled by an injury or a surgery, and gain access to soft tissue, bones, or the bloodstream.
In some cases, such as people with eczema, golden staph can also infect the skin itself, causing a variety of effects from boils to cellulitis.
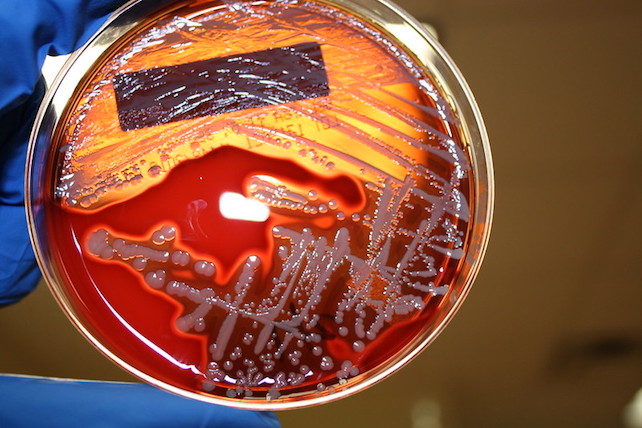
For the new study, researchers used a novel technique they developed called InToxSa (which stands for Intracellular Toxicity of S. Aureus). This let them study the behavior of golden staph inside human cells on a larger scale, they explain, with more speed and efficiency.
Led by University of Melbourne immunologist Abdou Hachani, the study suggests the key to stopping S. aureus from killing people might lie in learning more about how the bacteria stop our own immune systems from killing them.
"We tested hundreds of S. aureus strains taken from patients with bloodstream infections using InToxSa, and observed specific changes that make the bacteria less harmful and better at surviving in our bodies," Hachani says.
"We identified the genes that control the bacteria's ability to persist inside host cells without killing them," he adds. "This is an important advance to understand how S. aureus can cause lethal infections."
Golden staph is often considered an extracellular pathogen, the researchers write, which is a free-living microbe capable of causing disease without invading the cells of its host.
But it's not exclusively extracellular, they add, noting that golden staph can also survive and replicate inside its host's cells. This tactic may kill the host cells, but it helps the bacteria avoid detection by the host's immune system.
Using InToxSa, Hachani and his colleagues studied 387 golden staph strains from patients who had the species living in their blood. They identified specific mutations that make S. aureus less toxic to host cells and promote its "intracellular persistence," the researchers write.
"InToxSa is a powerful tool that combines genetic analysis, microbiological data, and statistical comparisons," explains co-author Tim Stinear, a molecular microbiologist at the University of Melbourne's Doherty Institute.
"It can handle a large volume of data in a systematic and standardized way, which eventually leads to more comprehensive and accelerated scientific discoveries – like ours," he says.
This kind of detail could help us better understand how golden staph gets away with wreaking so much havoc in the human body, the researchers note, which in turn might inspire better ways of preventing and treating infections.
That's especially important given the rise of tougher staph strains like methicillin-resistant Staphylococcus aureus, also known as MRSA, a major culprit behind the growing prevalence of hospital-acquired infections that can withstand even last-line antibiotics.
"Using this platform, we were able to identify mutations in the bacteria that are clinically relevant and promote their ability to persist inside the body," Stinear says. "This new knowledge will guide research to find new ways to combat these infections."
The study was published in eLife.