After 50 years of research, scientists have finally solved the mystery of how the foetal haemoglobin gene gets switched off in most people after birth. This huge finding could transform the way we treat several blood disorders affecting hundreds of thousands of people.
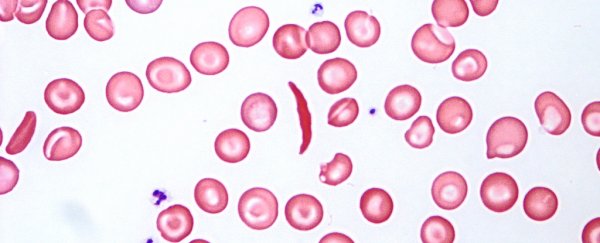
A number of disorders, such as sickle cell anaemia, are triggered by defective adult haemoglobin – the molecule that's crucial in picking up oxygen from the lungs and transporting it around the body.
A small minority of people naturally carry a genetic mutation that leaves the foetal haemoglobin gene activated after birth, which in turn helps reduce some of the symptoms associated with haemoglobin-related blood disorders.
Now scientists have worked out how to perform the same trick through CRISPR gene editing.
"It is organic because no new DNA is introduced into the cells," says senior researcher, molecular biologist Merlin Crossley from the University of New South Wales.
"Rather we engineer in naturally occurring, benign mutations that are known to be beneficial to people with these conditions."
The team found that the BCL11A and ZBTB7A genes were responsible for switching off the foetal haemoglobin gene because they bind directly to it.
Scientists had previously linked BCL11A to the foetal haemoglobin gene but this is the first time that experts how find evidence of how they interact – something researchers have been "competing furiously" to uncover, according to Crossley.
What's more, the team also identified how the natural mutations that keep the foetal haemoglobin gene active are able to disrupt this binding process.
Now that we understand more about how the globin (oxygen-transporting) genes are switched off - and have seen the team's encouraging CRISPR results - it looks like gene editing could provide improved treatments for a lack of haemoglobin in the blood system.
"It should prove to be a safe and effective therapy, although more research would be needed to scale the processes up into effective treatments," says Crossley.
While most adults have less than 1 percent of their foetal haemoglobin left in their systems, increasing its production has been shown to reduce some of the pain and fatigue associated with particular blood disorders.
So, if we can get the body to increase that production itself, the difference for those living with something like sickle cell anaemia could be significant.
In fact, foetal haemoglobin is even better at transporting oxygen around the body (which comes in handy before birth), and no toxic side effects have been observed when its production is ramped up in adult humans.
We already know that CRISPR can be used to copy and paste certain genes with a high level of accuracy – it's been used to tackle everything from fighting diseases to improving biofuels.
Now we've got another potential use of the gene editing technique that could improve the lives of hundreds of thousands of people – though, as the researchers note, we've still got a long way to go with this research before treatments can be developed.
"Our new approach can be seen as a forerunner to organic gene therapy for a range of common inherited blood disorders including beta thalassaemia and sickle cell anaemia," says Crossley.
The research has been published in Nature Genetics.