Self-organizing lumps of human brain tissue grown in the laboratory have been successfully transplanted into the nervous systems of newborn rats in a step towards finding new ways to treat neuropsychiatric disorders.
The 3D organoids, developed from stem cells to resemble a simplified model of the human cortex, connected and integrated with the surrounding tissue in each rat's cortex to form a functional part of the rodent's own brain, displaying activity related to sensory perception.
This, according to a team of researchers led by neuroscientist Sergiu Pașca of Stanford University, overcomes the limitations of dish-grown organoids, and gives us a new platform for modeling human brain development and disease in a living system.
"Most of the work that my lab has been doing has been motivated by this mission of trying to understand psychiatric disorders at the biological level so that we can actually find effective therapeutics," Pașca explained in a press briefing.
"Many of these psychiatric conditions, such as autism and schizophrenia, are likely uniquely human, or at least, they are anchored in unique features of the human brain. And the human brain has certainly not been very accessible, which has precluded the progress we've been making in understanding the biology of these conditions."
In 2008, scientists made a breakthrough: brain cells grown from induced pluripotent stem cells. Mature cells harvested from adult humans were reverse engineered (or induced) to return them to the 'blank' state of stem cells – the form cells take before they grow into cells with specializations, such as skin cells or cardiac cells.
These stem cells were then guided to develop into brain cells, which scientists cultivated to form lumps of brain-like tissue called organoids. These models of key areas of brain anatomy, such as the wrinkled outer cortex, could be used to study functions and development of brains up close.
As useful as they are, in vitro cortical organoids have limitations. Because they aren't connected to living systems, they don't complete maturation, depriving researchers of an opportunity to observe how they integrate with other major parts of a brain.
In addition, a brain organoid in a dish can't reveal the behavioral consequences of any defects scientists might identify. Since psychiatric disorders are defined by behavior, this stymies the ability to identify the physiological characteristics of these disorders.
In previous research, scientists have tried to overcome these hurdles by implanting human brain organoids into the brains of adult rats. Because of the developmental mismatch, the transplants didn't take: the developing neurons in the organoid couldn't form a strong connection with the fully developed network of an adult rat brain.
So Pașca and his colleagues tried something else: grafting the human brain tissue onto the brains of newborn rats, whose own brains have not yet developed and matured.
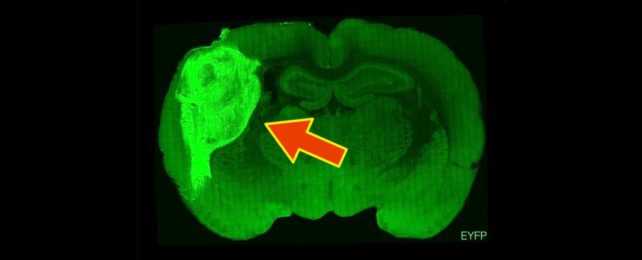
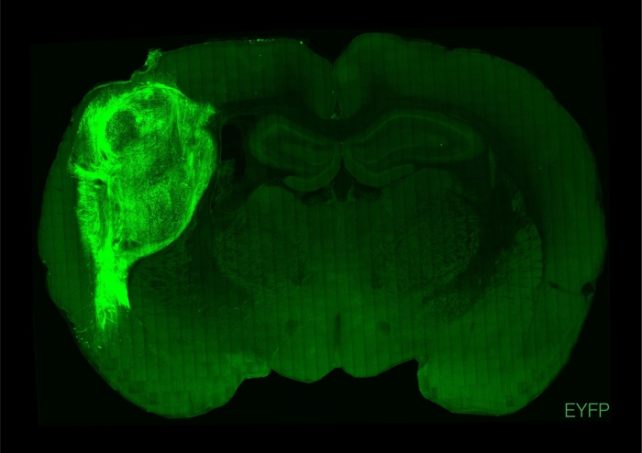
Human cortical organoids were cultured in a dish, and then transplanted directly into the somatosensory cortex (the area of the brain responsible for receiving and processing sensory information) of rat pups just a few days old. These rats were then left to grow into adults for another 140 days (rats are fully sexually mature between 6 and 12 weeks).
Then, the scientists studied the rats. They had genetically engineered the organoids to respond to blue light simulation, activating neurons when blue light is shone on them. This stimulation on the human neurons was performed while the rats were being trained to lick a spout to receive water. Later, when the blue light was shone on the organoids, the rats would automatically lick – displaying a response not seen in control groups.
This indicated that not only was the organoid functioning as part of the rat brain, it could help drive reward-seeking behavior.
Another group of neurons in the organoid showed activity when the scientist pushed the rats' whiskers – evidence that the neurons can respond to sensory stimulation.
Brain cells cultivated from three human patients with a genetic disease called Timothy syndrome were also used for some of the organoids. Timothy syndrome affects the heart, digits and nervous system, and usually results in early death.
After the behavioral tests, the rats were euthanized and their brains extracted and dissected, allowing the researchers to observe the integration of the organoids on a cellular level. They found the organoid neurons grew much larger than any neurons grown in vitro, extending into the rats' brains and forming networks with the native rat neurons.
The neurons in the rats with Timothy syndrome transplants showed less elaborate shapes, and formed different synaptic connections with the surrounding brain tissue compared to control groups. This is a new discovery, and could not have been discovered in a brain organoid in a dish.
Although the platform still has some limitations, the team believes that it has the potential to become a powerful new tool for understanding brain development and disease.
"Overall, this in vivo platform represents a powerful resource to complement in vitro studies of human brain development and disease," the authors write in their paper.
"We anticipate that this platform will allow us to uncover new circuit-level phenotypes in patient-derived cells that have otherwise been elusive and to test novel therapeutic strategies."
The research has been published in Nature.