By reprogramming aggressive cancerous cells so they mature into harmless immune cells known as macrophages, scientists in the US say they might have found a way to not only neutralise the potentially fatal disease, but also use it against itself.
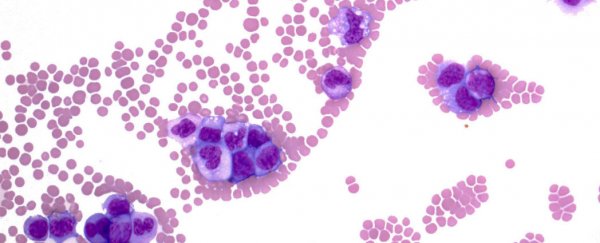
Acute lymphoblastic leukemia (ALL) is an acute form of leukaemia that affects the body's lymphocyte-forming white blood cells called lymphoblasts. It's an extremely aggressive and fast-moving type of cancer, causing an overproduction of defective lymphoblasts that, instead of producing an immune response, never mature.
These stunted lymphoblasts actively halt the production of vital cells, including red and white blood cells and platelets, moving from the bone marrow to other organs, eventually wreaking havoc on a person's entire body. The disease is most commonly found in children between the ages of two and five, and the elderly, and while the prognosis has certainly improved for patients over the past five decades, it can be fatal. In developing countries, there's a five-year survival rate in more than 85 percent of diagnosed patients, which means about eight in 10 patients manage to survive at least five years past diagnosis.
As with any type of cancer, treatment is not particularly pleasant, and is especially hard on the children it afflicts. Combinations of chemotherapy, steroids, and radiation therapy are common, and there are no surgical options, because of how widespread the cancer cells become.
But there is hope that a new form of drug could change the way we treat leukaemia, thanks to a discovery by a team from the Stanford University School of Medicine. As many of the best scientific discoveries are, this one was made by accident, when the researchers were doing their best to keep some leukaemia cells alive in a petri dish so they could continue to study their behaviour.
These were precursor B-cell lymphoblastic leukaemia cells (B-ALL), which cause the most common type of ALL; about 85 percent of children with ALL have the B-ALL form. "We were throwing everything at them to help them survive," lead researcher and assistant professor of medicine, Ravi Majeti, said in a press release.
One of the team, Scott McClellan, noticed that some of the leukaemia cells were morphing into different sizes and shapes, and eventually started to resemble macrophages - the cells they would have become had they not remained stunted and cancerous. Looking back at previous research in which a separate team managed to alter the growth of leukaemia cells in mice, the team soon realised that cancerous lymphoblasts could be forced into mature, harmless macrophages when combined with certain types of proteins that altered their genetic activity.
Using these proteins, the team replicated the results of the previous mouse study using human cancer cells. They successfully transformed them into macrophages, and these macrophages went on to 'eat' any cancer cells and pathogens the researchers threw at them. They've even proven to be especially good at fighting leukaemia cells themselves, Majeti said. "Because the macrophage cells came from the cancer cells, they will already carry with them the chemical signals that will identify the cancer cells, making an immune attack against the cancer more likely."
The results have been published in the Proceedings of the National Academy of Sciences:
"We show here that cancerous cells from B-ALL patients can be reprogrammed, causing them to change into cells that resemble normal macrophages and can perform macrophage-associated functions such as the consumption of bacteria.
Importantly, unlike typical B-ALL cells, these reprogrammed cells are no longer able to cause disease in immunodeficient mice. Finally, we show that this reprogramming process may occur to some degree in patients with B-ALL. This indicates that reprogramming B-ALL cells into macrophages might represent a previously unidentified therapeutic strategy."
The next step is to develop a drug that can prompt the transformation of the lymphoblasts on its own. One option is an existing cancer drug - Retinoic acid - which is used to turn cancer cells into mature cells called granulocytes. Perhaps it could be used to induce the same transformation in leukaemia patients too.