Scientists have developed a specially engineered biochip that uses electricity to heal wounds up to three times faster than normal.
It's well known that electric fields can guide the movements of skin cells, nudging them towards the site of an injury for instance. In fact, the human body generates an electric field that does this naturally. So researchers from the University of Freiburg in Germany set out to amplify the effect.
While it might not heal severe injuries with the speed of a Marvel superhero, it could radically reduce the time it takes for small tears and lacerations to recover.
For people with chronic wounds that take a long time to heal, such as in elderly folk, those with diabetes, or people with poor blood circulation, recovering quickly from frequent small, open cuts could be a literal lifesaver.
"Chronic wounds are a huge societal problem that we don't hear a lot about," says Maria Asplund, a bioelectronics scientist at the University of Freiburg and Chalmers University of Technology in Sweden.
"Our discovery of a method that may heal wounds up to three times faster can be a game changer for diabetic and elderly people, among others, who often suffer greatly from wounds that won't heal."
While it's established electricity can assist healing, the impact of an electric field's strength and direction on the process has never been well established.
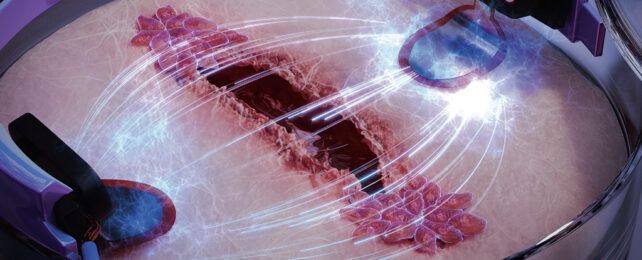
So the researchers developed a bioelectronic platform and used it to grow artificial skin made up of cells called keratinocytes, which are the most common skin cell type and crucial for the healing process.
They also compared the application of electric fields on one side of the wound with alternating fields on both sides of the wound.
Both healthy keratinocytes and keratinocytes designed to resemble those in people with diabetes migrated up to three times faster than skin cells without any electrical interference, with an electrical push from just one side of the wound proving most effective at repairing the artificial skin in the quickest time. Fortunately, none of the cells were damaged by the electrical fields tested.
"We saw that when we mimic diabetes in the cells, the wounds on the chip heal very slowly," says Asplund. "However, with electric stimulation, we can increase the speed of healing so that the diabetes-affected cells almost correspond to healthy skin cells."
Wounds that won't heal in a typical, rapid fashion raise the risk of infection setting in and delaying healing further. In the most severe cases, this can lead to amputation, making any process that speeds up the process worth investigating for patients and healthcare providers.
The next stage is testing how all of this works on actual wounds in living humans, rather than skin cells grown in the lab. Developing practical applications will rely on translating the cheap, readily-available used materials in the experiment to real-world situations.
"We are now looking at how different skin cells interact during stimulation, to take a step closer to a realistic wound," says Asplund. "We want to develop a concept to be able to 'scan' wounds and adapt the stimulation based on the individual wound."
"We are convinced that this is the key to effectively helping individuals with slow-healing wounds in the future."
The research has been published in Lab on a Chip.