Getting drugs to targeted areas of the body has always been a struggle for medicine. Either the drugs can't find an efficient pathway, or they end up killing a whole lot of healthy cells along the way. But this could all be about to change, because scientists are now growing smart nanocrystals that could be used to direct drugs to the right spot.
Current cancer treatments affect both tumour cells and rapidly regenerating healthy cells, such as hair follicles and bone marrow, which causes the awful side effects associated with chemotherapy and other cancer drugs.
"At this stage the treatment for cancer is applying radiation or chemical drugs which tends to be very aggressive," said lead researcher Dayong Jin from the University of Technology Sydney (UTS) Faculty of Science. "You might kill the cancer cells, but you can also kill up to 70 to 90 percent of the healthy cells."
This targeting problem is also what causes difficulty in treating neurological diseases such as Parkinson's. The blood-brain barrier is a very effective way to keep out viruses and other unwanted particles, but makes drug delivery to the brain difficult. "A lot of the time the drug tends to circulate in the blood system and not the brain," said Jin.
Another issue is that many drugs and drug delivery methods are not able to escape our immune system- the medication often ends up being devoured by macrophages or other white blood cells. This means we're currently using more drugs than we need, and they're not working as effectively as they should be.
But these new nanocrystals could change all of that - they can be designed with many different properties, and are able to blend in to avoid triggering an immune response. "We need to find a new vehicle for drug delivery that allows the healthy cells and blood-brain barrier to recognise the drug as a friend and not an enemy," said Jin.
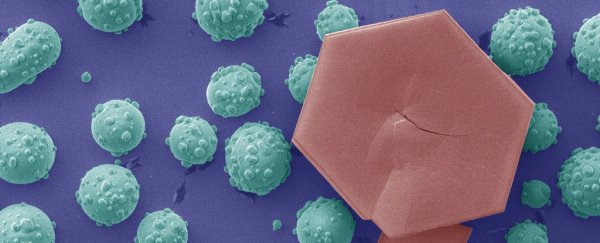
Jin and his team have been working to find a way to efficiently create these new vehicles. Over the past three years, they've created a library of their nanocrystal creations, all shaped differently due to how their atoms cluster together. Each one acts as a different molecular tag, and can be used in different ways – such as to deliver drugs, target specific cells, and even help to image the body for doctors.
To create the crystals, the researchers introduced different ratios of oleate anions and molecules to the crystal formation. The different ratios change the structures, and create the ability to graft shells over the different nanocrystals.
These shells can then be used for a wide variety of purposes, whether it's targeting the brain and moving through the blood-brain barrier, or attaching to a florescent protein, which allows us to see a tumour using real-time imaging.
"Hybrid nanocrystals are multifunctional and able to do different things simultaneously. For example, one can design a super nanoparticle that has optical, magnetic and chemical responses which allows for multiple modality imaging of the disease and [eventually] super high resolution images," said Jin.
Nanocrystals with that many functions means they would be highly effective at seeking out and then showing you whatever you wanted. Whether that's a tumour that needs to be cut out, or an area of the brain that's been damaged.
"Having precise diagnostics is also important because when a surgeon operates they need to understand exactly where the tumour is," said Jin. "If higher resolution imaging is available, the surgeon will be able to see a precise boundary between the healthy cells and the tumour cells which will result in a better outcome for the patient."
We'll be watching the progress closely. Here's hoping that nanocrystals can help make the brutal side effects of chemotherapy a thing of the past.
This research has been published in Nature Communications.
UTS Science is a sponsor of ScienceAlert. Find out more about their research.