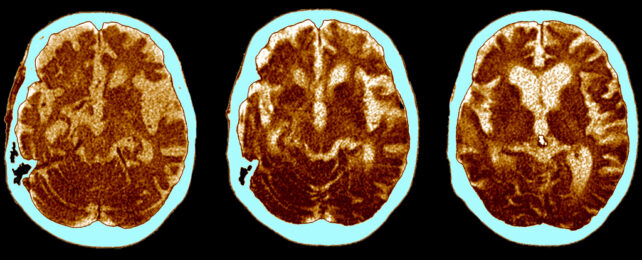
Some people have the changes consistent with Alzheimer's without presenting any symptoms, almost as if their brains are more resistant to the condition. A new study has explored how this perplexing phenomenon might point the way to treatments.
A team of researchers led by scientists from the Netherlands Institute for Neuroscience looked at brain tissue samples stored at the Netherlands Brain Bank, a repository of donated brains from more than 5,000 people who died with a brain disease.
Among those thousands of samples, the team found just 12 who had been cognitively healthy prior to their death yet had clear neurological signs of the disease's underlying pathology.
Beyond demonstrating just how rare it is for brains to avoid the debilitating effects of Alzheimer's, the small sample gave the team an opportunity to learn what might make such brains so resilient.
"What is happening in these people at a molecular and cellular level wasn't clear," says Luuk de Vries, a neuroscientist from the Netherlands Institute for Neuroscience. "We therefore searched for donors with brain tissue abnormalities who did not show cognitive decline in the Brain Bank."
This kind of resilience has been noted before, and it's thought that both the genetics we're born with and the lifestyle choices we make might have some effect. These different factors are tied to the development of Alzheimer's in general as well.
By analyzing the unique combinations of hundreds of genes being expressed within cognitively healthy Alzheimer's brains, brains of more typical Alzheimer's patients, and otherwise healthy controls without the disease, researchers found key differences in the resilient brains related to the astrocyte cells that are involved with the clearing of waste out of the brain.
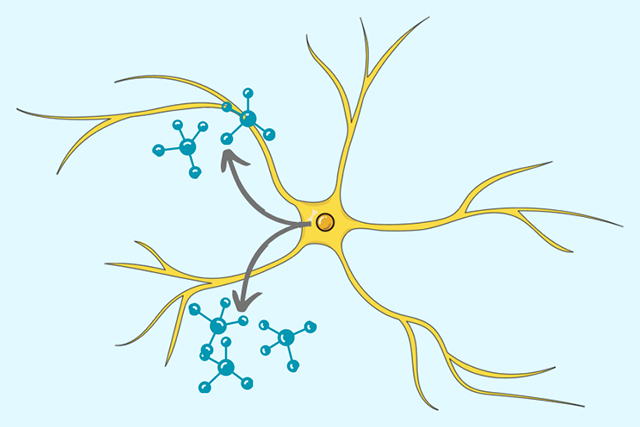
What's more, the resilient brains seemed to be better at removing toxic proteins associated with the development of Alzheimer's. It seems these brains are somehow better at stopping neurological garbage from building up.
Another difference was more efficient energy production in the cells in resilient brains. It's not clear yet what's behind these differences or how they link in to Alzheimer's disease, but identifying what the differences are is an important first step.
"If we can find the molecular basis for resilience, then we have new starting points for the development of medication, which could activate processes related to resilience in Alzheimer's patients," says de Vries.
Alzheimer's now affects some 47 million people worldwide, and those numbers are rising rapidly. We're still not sure what combination of factors are required for the degeneration to progress, how to prevent the disease from arising, or how its damage could be reversed – but every study like this one gets us closer to some answers.
The next step with this particular research is to try and figure out why there are these differences in the production processes of resilient brains. From there, it might be possible to develop drugs that help make brains better able to protect themselves.
"It remains difficult to determine from human data which process initiates the disease process," says de Vries. "You can only demonstrate this by changing something in cells or animal models and seeing what happens next. That is the first thing we have to do now."
The research has been published in Acta Neuropathologica Communications.