After veteran Tony Macie came back from Iraq in 2007, he was diagnosed with post traumatic stress disorder (PTSD). Macie went to the Veterans Health Administration (VA) 'on and off' and tried the standard therapy.
"And then I kind of just fell off the radar, secluded, and did my own thing and got really dependent on a lot of the meds," Macie explains in a video by the Multidisciplinary Association for Psychedelic Studies (MAPS).
The retired sergeant then became part of a clinical trial organised by MAPS that was testing an unusual substance in an attempt to heal people who hadn't responded to traditional therapies for PTSD.
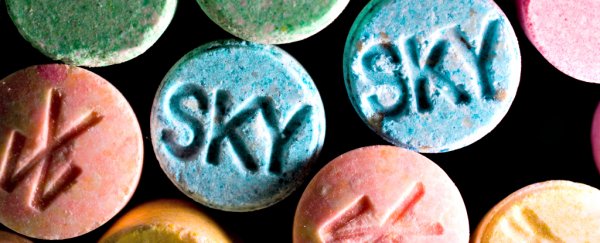
That substance, MDMA (commonly referred to as 'Molly'), is the pure form of something commonly thought of as an illegal party drug – ecstasy. (Most non-research substances that are sold as ecstasy or Molly are not actually pure MDMA and can be significantly more dangerous.)
The trial pairs MDMA with psychotherapy.
"One of the first things I said when it kicked in was 'this is what I've been looking for,'" Macie says in the video. "I reconnected with myself and did a lot of internal work, and afterwards it was like a huge weight was lifted off my shoulders."
The trial Macie was involved in and other Phase 2 clinical studies conducted by MAPS have been so effective that the Food and Drug Administration (FDA) agreed on Tuesday to allow large-scale Phase 3 clinical trials – the third and final in the three sets of human trials required before the FDA will consider a new drug for approval – to go forward, according to a report in the New York Times.
If those trials continue to show that MDMA effectively treats PTSD, ecstasy could enter clinical use as soon as 2021, fitting the timeline that MAPS has been working towards for some time now.
And so far, MDMA has consistently been very effective.
One of the early studies conducted by MAPS showed that 83 percent of the study participants no longer showed signs of PTSD two months after treatment, and long-term follow-ups conducted an average of four years later showed that most of those benefits stuck.
That was a proof-of-concept study, with just 20 participants, all of whom had psychotherapy as well. (Twelve were given MDMA, and eight were given a placebo; 25 percent of those on the placebo improved, too.)
Though small and preliminary, the results were encouraging enough to help lead to Phase 2 clinical trials, which MAPS announced were coming to an end last March.
These trials consisted of at least eight studies that Brad Burge, the director of communications for MAPS, recently told Inverse treated 136 people using MDMA-assisted psychotherapy for PTSD.
Those trials dealt with patients who were struggling with PTSD from a variety of sources. They included military veterans, people who had been sexual assaulted, firefighters, and police officers, all who had not responded to traditional treatments.
The data released from those studies so far is very promising, with a large percentage of patients not showing any signs of PTSD more than a year after completing the therapy.
"We can sometimes see this kind of remarkable improvement in traditional psychotherapy, but it can take years, if it happens at all," Michael C. Mithoefer, one psychiatrist involved in the research, told The Times.
The final tests will involve hundreds of people and must be conducted before the FDA decides to approve a new medication. MAPS has applied for 'breakthrough' therapy status, which could speed up the approval process.
"Phase 3 starts around 2017, and it will take four to five years to finish. So that will put it at early 2021 for FDA approval," Burge has previously said.
MAPS is mostly raising money themselves to fund what they describe as a roughly US$20 million plan to complete these trials, which are largely not of interest to pharmaceutical companies since the patent on MDMA has expired. That will mean significant fundraising is required.
Last year, the organisation reported US$9.1 million in assets; more than US$5 million of that is a bequest from a longtime board member that has been earmarked specifically for those Phase 3 trials.
In fiscal year 2015, MAPS raised a total of US$2.99 million from 2,500 donors. It noted in its most recent annual report that "substantially increasing our donor base" will be necessary to to move forward with Phase 3 trials.
It's only after those trials wrap up that we'll know for sure whether using MDMA to treat PTSD is safe and effective. MAPS calls making that happen its "top priority".
The group is also conducting research testing the efficacy of MDMA-assisted therapy to treat social anxiety in autistic adults and to treat anxiety associated with life-threatening illnesses like cancer.
"It's a really interesting and a very powerful new approach," former National Institute of Mental Health director Thomas Insel told the San Francisco Chronicle.
"It's not just taking MDMA. It's taking it in the context of a treatment that involves improved insight and increased skills and using this in the broader context of psychotherapy."
As Macie says in the MAPS video, "this tool, it may not be the end all, but it [could] be a tool that can help a lot of people drastically".
This article was originally published by Business Insider.
More from Business Insider: