As a psychiatrist, I find that one of the hardest parts of my job is telling parents and their children that they are not to blame for their illness.
Children with emotional and behavioral problems continue to suffer considerable stigma. Many in the medical community refer to them as "diagnostic and therapeutic orphans". Unfortunately, for many, access to high-quality mental health care remains elusive.
An accurate diagnosis is the best way to tell whether or not someone will respond well to treatment, though that can be far more complicated than it sounds.
I have written three textbooks about using medication in children and adolescents with emotional and behavioural problems. I know that this is never a decision to take lightly.
But there's reason for hope. While not medically able to diagnose any psychiatric condition, dramatic advances in brain imaging, genetics and other technologies are helping us objectively identify mental illness.
Knowing the signs of sadness
All of us experience occasional sadness and anxiety, but persistent problems may be a sign of a deeper issue. Ongoing issues with sleeping, eating, weight, school and pathologic self-doubt may be signs of depression, anxiety or obsessive-compulsive disorder.
Separating out normal behaviour from problematic behaviour can be challenging. Emotional and behaviour problems can also vary with age.
For example, depression in pre-adolescent children occurs equally in boys and girls. During adolescence, however, depression rates increase much more dramatically in girls than in boys.
It can be very hard for people to accept that they – or their family member – are not to blame for their mental illness. That's partly because there are no current objective markers of psychiatric illness, making it difficult to pin down.
Imagine diagnosing and treating cancer based on history alone. Inconceivable! But that is exactly what mental health professionals do every day.
This can make it harder for parents and their children to accept that they don't have control over the situation.
Fortunately, there are now excellent online tools that can help parents and their children screen for common mental health issues such as depression, anxiety, panic disorder and more.
Most important of all is making sure your child is assessed by a licensed mental health professional experienced in diagnosing and treating children.
This is particularly important when medications that affect the child's brain are being considered.
Seeing the problem
Thanks to recent developments in genetics, neuroimaging and the science of mental health, it's becoming easier to characterise patients. New technologies may also make it easier to predict who is more likely to respond to a particular treatment or experience side effects from medication.
Our laboratory has used brain MRI studies to help unlock the underlying anatomy, chemistry and physiology underlying OCD.
This repetitive, ritualistic illness – while sometimes used among laypeople to describe someone who is uptight – is actually a serious and often devastating behavioral illness that can paralyse children and their families.
Through sophisticated, high-field brain imaging techniques – such as fMRI and magnetic resonance spectroscopy – that have become available recently, we can actually measure the child brain to see malfunctioning areas.
We have found, for example, that children 8 to 19 years old with OCD never get the "all clear signal" from a part of the brain called the anterior cingulate cortex. This signal is essential to feeling safe and secure.
That's why, for example, people with OCD may continue checking that the door is locked or repeatedly wash their hands. They have striking brain abnormalities that appear to normalise with effective treatment.
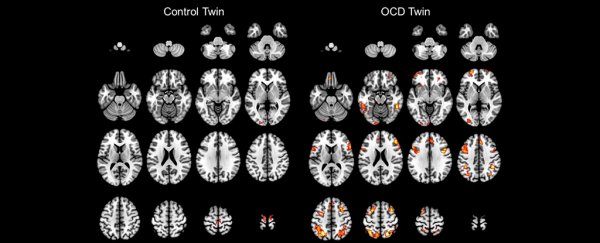
We have also begun a pilot study with a pair of identical twins. One has OCD and the other does not. We found brain abnormalities in the affected twin, but not in the unaffected twin.
Further study is clearly warranted, but the results fit the pattern we have found in larger studies of children with OCD before and after treatment as compared to children without OCD.
Exciting brain MRI and genetic findings are also being reported in childhood depression, non-OCD anxiety, bipolar disorder, ADHD and schizophrenia, among others.
Meanwhile, the field of psychiatry continues to grow. For example, new techniques may soon be able to identify children at increased genetic risk for psychiatric illnesses such as bipolar disorder and schizophrenia.
New, more sophisticated brain imaging and genetics technology actually allows doctors and scientists to see what is going on in a child's brain and genes.
For example, by using MRI, our laboratory discovered that the brain chemical glutamate, which serves as the brain's "light switch," plays a critical role in childhood OCD.
What a scan means
When I show families their child's MRI brain scans, they often tell me they are relieved and reassured to "be able to see it".
Children with mental illness continue to face enormous stigma. Often when they are hospitalised, families are frightened that others may find out. They may hesitate to let schools, employers or coaches know about a child's mental illness.
They often fear that other parents will not want to let their children spend too much time with a child who has been labeled mentally ill. Terms like "psycho" or "going mental" remain part of our everyday language.
The example I like to give is epilepsy. Epilepsy once had all the stigma that mental illness today has. In the Middle Ages, one was considered to be possessed by the devil.
Then, more advanced thinking said that people with epilepsy were crazy. Who else would shake all over their body or urinate and defecate on themselves but a crazy person? Many patients with epilepsy were locked in lunatic asylums.
Then in 1924, psychiatrist Hans Berger discovered something called the electroencephalogram (EEG). This showed that epilepsy was caused by electrical abnormalities in the brain. The specific location of these abnormalities dictated not only the diagnosis but the appropriate treatment.
![]() That is the goal of modern biological psychiatry: to unlock the mysteries of the brain's chemistry, physiology and structure.
That is the goal of modern biological psychiatry: to unlock the mysteries of the brain's chemistry, physiology and structure.
This can help better diagnose and precisely treat childhood onset mental illness. Knowledge heals, informs and defeats ignorance and stigma every time.
David Rosenberg, Professor, Psychiatry and Neuroscience, Wayne State University.
This article was originally published on The Conversation. Read the original article.