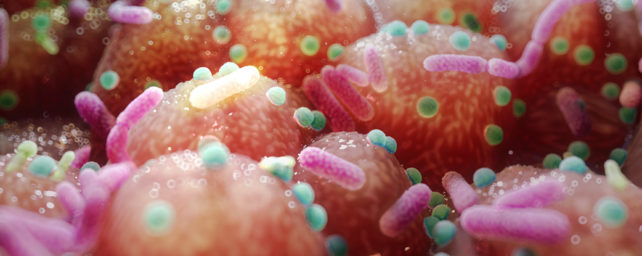
Scientists have discovered DNA-damaging molecules made by gut bacteria that may help explain why people with inflammatory bowel disease (IBD) have higher rates of colorectal cancer than those without the condition.
In a new study, published Thursday (27 October) in the journal Science, researchers identified a previously unknown class of DNA-damaging molecules, or genotoxins, that they named the "indolimines."
These molecules are produced by Morganella morganii, a bacterium that proliferates in the guts of patients with IBD and those with colorectal cancer.
Indolimines damaged DNA in lab dish experiments and also drove cancer growth in mice with colorectal tumors.
And by blocking the production of indolimines by M. morganii, the scientists found that they could prevent tumor growth in the mice.
Other gut bugs have been linked to IBD and colorectal cancer in the past, said Cynthia Sears, a professor of medicine and oncology at the Johns Hopkins University School of Medicine in Baltimore, who was not involved in the study.
For example, select strains of Escherichia coli are associated with IBD and make a genotoxin called colibactin, which damages DNA and drives tumor growth in mice.
The new study adds to our understanding of how other bacteria might contribute to these diseases.
Related: Antibiotics may raise colon cancer risk, massive study suggests
"We have a vast array of data – and this is just one other piece that's been added to that – that links the microbiome to colon diseases and colon cancer," Sears said.
In the long term, this line of research could lead to screening tools that help doctors identify patients at high risk of colon cancer, simply by taking a poop sample.
It could also lead to preventative treatments that reduce the abundance of cancer-linked bacteria in patients' guts and thus lower their risk of disease.
At this point, "we certainly know those clinical associations, but we don't know how to prevent them, or disrupt them, to decrease the risk of cancer," Sears said.
"We need to figure out at a molecular level what the mediators are so we can bring something to the bedside, for patients."
To spot the mysterious DNA-damaging molecules, researchers first screened more than 100 types of gut bacteria from the stool samples of 11 IBD patients. (IBD is a term that includes ulcerative colitis, which causes inflammation and sores in the lining of the colon and rectum, and Crohn's disease, which causes inflammation in all or part of the digestive tract, most commonly in the small intestine.)
The team grew each of these bacterial strains in a lab dish with DNA and identified 18 strains that damaged the genetic molecule.
From these strains, the scientists identified individual molecules that the bacteria produced and tested which ones caused DNA damage.
Interestingly, the DNA damage that the researchers observed did not match that caused by colibactin, and the flagged bacteria were incapable of making colibactin.
"These data thus implied the existence of previously unrecognized microbiota-derived genotoxins," the researchers wrote in their report.
To characterize some of the unknown genotoxins, the researchers zoomed in on M. morganii, which was previously reported to be prevalent in both IBD and colon cancer patients' guts.
Through this work, they not only discovered the indolimines, but also identified a bacterial gene required to make them: the so-called aspartate aminotransferase (aat) gene, which codes for an enzyme.
Related: People who live to 100 have unique gut bacteria signatures
In a mouse model of colorectal cancer, M. morganii strains with the aat gene exacerbated tumor growth.
But by deleting this gene from the bacteria, the team stopped indolimines from being made and thus halted the cancer growth.
"The best evidence they present is the mouse studies – that's what convinced me," Sears said.
However, the mouse model has its limitations. The researchers used "gnotobiotic" mice, meaning they picked exactly which bacteria would grow in the rodents; they included only M. morganii and seven other bacteria that weren't genotoxic.
This allowed the scientists to observe the cancer-driving effects of M. morganii, but didn't capture the complexity of a natural gut microbiome, Sears said.
More work is needed to understand how prevalent M. morganii is in different types of IBD and colorectal cancer.
Follow-up studies will also need to pinpoint exactly how indolimines cause DNA damage and how influential these molecules are over cancer development, compared with other genotoxins, Sears said.
"This is a first step," she said of the new paper.
Related content:
- Experimental rectal cancer drug caused all patients' tumors to disappear in small trial
- The same exact foods affect each person's gut bacteria differently
- Gut bacteria may 'talk' to the brain, mouse study suggests
This article was originally published by Live Science. Read the original article here.