Every single cell in your body ticks to the rhythm of its own internal clock – even cancerous ones.
Timing chemotherapy with these 24-hour (ish) circadian cycles could significantly improve treatments, according to research at Europe's largest university hospital, the Charité in Berlin, Germany.
When treating the cells of triple-negative breast cancer – a highly aggressive and hard-to-treat disease – researchers found the effectiveness of one chemotherapeutic drug differed by up to 30 percent depending on when the medicine was administered to certain cell lines.
"Overall, our findings indicate that personalized treatment plans based on individual circadian rhythms could substantially improve the efficacy of cancer treatment," concludes computational biologist Adrián Enrique Granada from the Charité Comprehensive Cancer Center (CCCC).
The internal clock of a cell is made up of clock-controlled genes and protein feedback loops that keep the unit in sync with the rest of the body.
Core 'clock' genes code for proteins in the cell, which are expressed rhythmically throughout the day, determining the cell's metabolism, proliferation, immune response, DNA repair, and even its death.
Each clock in each cell is wound up differently depending on the tissue in which it lives. The circadian clock among liver cells, for instance, is highly tuned to meals, while the daily cycle among brain cells is highly tuned to light.
Cancerous cells also have their own internal clock, and depending on the type, they may grow and divide at different times of day.
In 2022, for instance, a study found that breast cancer cells from human patients divide and spread at night at higher rates.
What's more, a study published earlier this year found that the 24-hour circadian clock cycle can impact the strength of tumor defenses, and the ability of medicine to get past those defenses.
Understanding how cellular clocks impact disease progression is an emerging field of scientific research. "Yet, uncovering the optimal treatment timings remains challenging," explain cell biologist Carolin Ector, from CCCC, and her colleagues from institutes in Germany and Luxembourg.
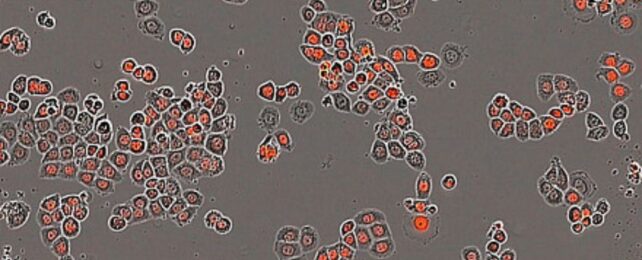
Together, the researchers have introduced a new way to model and monitor living cells and their circadian rhythms, growth, and drug responses.
The team calls their method the "chronotherapeutic index", and it essentially determines at what time of day it is best to deliver medicine.
The screening process works for numerous cell types, including non-malignant skin cancer cells and malignant bone cancer cells. But researchers have showcased the potential of the approach using triple negative breast cancer cells.
Ultimately, their screening method identified 80 distinctly different cancer cell responses depending on when the chemotherapeutic drugs 5-fluorouracil, cisplatin, and doxorubicin were applied across the different cancer cell lines.
For one particular lineage of breast cancer cells, chemotherapy had the highest overall benefit at 10 to 12 hours into the 24-hour (ish) cell cycle and 18 to 20 hours into the cycle. Earlier treatment times yielded minimum benefit.
Applied to this same cell line, the chemotherapy drug 5-FU showed a "clear preference for administration" between 8 and 10 hours into a cycle, whereas torin and paclitaxel showed more variability in their maximum and minimum benefit times.
By contrast, two other cell lines of breast cancer showed maximum treatment benefits throughout the day. In other words, it didn't matter as much when chemotherapy drugs were administered.
The research was only conducted among cells, but researchers hope their new index will pave the way for future cancer treatments.
"We're also planning to study the molecular mechanisms behind the circadian influences on medication sensitivity to further optimize treatment times and identify new therapeutic targets," says Granada.
The study was published in Nature Communications.