An experiment on model brains has added more evidence to the hypothesis that the viruses responsible for chickenpox and herpes can team up to cause Alzheimer's disease.
While the claim continues to be fiercely debated, researchers at Tufts University and The University of Oxford argue they have just demonstrated the presence of two viruses in tandem can promote an excess of proteins responsible for Alzheimer's characteristic brain plaques.
A potential link between the cold-sore virus, herpes simplex (HSV-1), and Alzheimer's has already received attention over the years. Not only has its DNA been found in high amounts in the brains of elderly people, those who have a gene associated with Alzheimer's can have a heightened risk of developing the condition if they also have HSV-1.
Similar to herpes virus, the chicken pox virus varicella-zoster can lay dormant in nerve cells for years, emerging later in life to wreak havoc as shingles.
It's possible the resulting inflammation could raise the risk of dementia, yet shingles rarely erupts more than once or twice in a lifetime. Hardly enough, it was thought, to cause Alzheimer's.
Yet there are good reasons to suspect the two conditions are somehow linked. Population studies in Taiwan, the UK, South Korea, and the US suggest that vaccination against the reemergence of the varicella-zoster virus as shingles lowers the risk of dementia, for example.
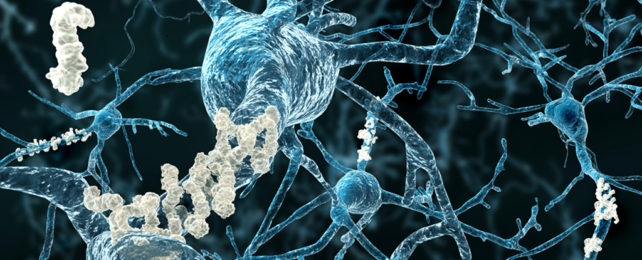
To get a better idea of what might be going on, the researchers built a brain-like environment within six-millimeter-wide, doughnut-shaped sponges made of silk protein and collagen. These were populated with stem cells that grew into functional neurons and supporter tissues called glial cells, which helped keep the neurons alive and well.
When the model brain tissue was infected with varicella-zoster alone, there were no signs of an increase in the signature Alzheimer's proteins tau and beta amyloid.
But if the neurons already contained a dormant herpes simplex virus, the exposure to the varicella-zoster virus led to a reactivation of the herpes virus.
This twin-pronged attack was followed by a dramatic increase in the tau and beta-amyloid proteins associated with Alzheimer's disease, as well as a slowdown in the neurons' signals.
"It's a one-two punch of two viruses that are very common and usually harmless, but the lab studies suggest that if a new exposure to varicella-zoster virus wakes up dormant herpes simplex virus, they could cause trouble," says lead author, biomedical engineer Dana Cairns from Tufts University.
Beta-amyloid proteins can collect in the brain as plaques, which are abnormal clusters of protein fragments that disrupt nerve signaling. Tau is a protein that usually keeps microtubules in straight lines. In people with dementia, tau becomes faulty and the microtubules start to twist and tangle, starving cells of nutrients.
Just how these two proteins might be involved with Alzheimer's is itself a matter of ongoing debate, with drugs targeting plaque formation failing to live up to expectations. Yet the fact they are a feature of the condition makes them a clear signal that something has gone awry.
Some experts not involved in the study have cautioned that the experiment does not conclusively demonstrate that this interaction is what causes Alzheimer's disease because building a brain-like tissue outside the human body is a pretty artificial environment.
They argue that it is the inflammation, a byproduct of the viral infection, not the specific virus itself that's triggering the problem, so other viruses could be just as implicated in the disease.
"These are laboratory findings and do not directly implicate these viruses as the main cause of Alzheimer's disease, but the results are important and should continue to stimulate research," says Paresh Malhotra, a neurologist at Imperial College London.
Future studies will almost certainly unravel the roles viruses play in the complex series of events that leads to the degeneration of nerves responsible for Alzheimer's symptoms.
"We know there is a correlation between HSV-1 and Alzheimer's disease, and some suggested involvement of varicella-zoster virus, but what we didn't know is the sequence of events that the viruses create to set the disease in motion," says biomedical engineer David Kaplan at Tufts University and the senior author on the paper.
"We think we now have evidence of those events."
This paper was published in the Journal of Alzheimer's Disease.