Most people with type 1 diabetes cannot reverse their autoimmune disease or put it into spontaneous remission – all they can do is manage their blood sugar levels with insulin, a healthy diet, and regular exercise.
Now, the successful treatment of the condition in a young woman in China has brought the possibility of a universal cure tantalizingly close.
In June 2023, doctors injected the equivalent of roughly 1.5 million insulin-producing cells into the patient's abdominal muscles. The community of cells was carefully reprogrammed from her own stem cells.
Two and a half months later, the woman's lifelong dependence on injected insulin came to an end – completely reversing her long-term, hard-to-control diabetes.
More than four months after the transplantation, her body was producing enough insulin on its own to keep her in a safe blood glucose range for more than 98 percent of the day.
If this one patient can keep producing insulin naturally in the coming years, she could one day be declared 'cured' – the first successful case of its kind in the scientific literature.
"That's remarkable," diabetes researcher Daisuke Yabe, who was not involved in the research, told Nature reporter Smriti Mallapaty.
"If this is applicable to other patients, it's going to be wonderful."
Researchers in China are already planning to open up their trial to new patients.
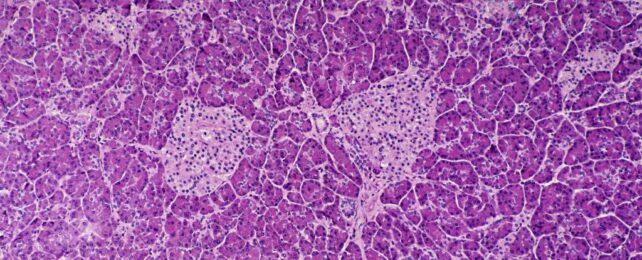
Type 1 diabetes occurs when the body's immune system attacks clusters of cells in the pancreas that produce insulin, called islets.
Transplanting islets or an entire pancreas from a donor to a patient with type 1 diabetes can prove curative in some selective cases, but it is an extreme and potentially dangerous option, and there are too few donors to make it accessible for the millions of those with this autoimmune disease worldwide.
For over two decades now, scientists have tried to coax cells from fully-developed adult tissue types back into a blank state known as an induced pluripotent stem cell, and in turn, transform them into insulin-producing cells.
Figuring out how to do that with accuracy, however, is tricky work. The final product doesn't always match real pancreatic islets.
Researchers in China have taken a new route that they say allows them greater control. Instead of introducing proteins to the stem cells, which trigger certain gene expressions, reprogramming the adult tissues into the blank state, the team has engineered induced pluripotent stem cells using small molecules.
After testing the technique in mice and non-human primates with success and safety, the team of researchers got their approval for a human clinical trial. The trial is ongoing, and three people are currently enrolled.
One of those patients is a 26-year-old woman, who was diagnosed with type 1 diabetes at age 14, and her results from one year in the trial have now been published.
Previously, this patient had already had a pancreas transplant for severe hypoglycemia, but the organ had to be removed due to "severe thrombotic complications".
So far, her stem cell transplant seems to be working better, alongside her immunosuppressive drugs.
The findings join several other recent clinical trials that suggest further studies on stem cell transplantations are warranted.
In a trial in the US, for instance, a dozen patients with type 1 diabetes were injected with islets, created from donated stem cells. The group was also treated with immunosuppressants. All 12 participants began producing insulin naturally when glucose entered their bloodstream, according to preliminary results.
"Overall," write the researchers in China, "the findings support further clinical studies in this direction and mark a step forward in achieving the potential of personalized cell therapy… to treat disease."
The study was published in Cell.