A trial testing how long a teaspoon-sized transfusion of lab-grown red blood cells lasts in the body could revolutionize clinical care for people with blood disorders who require regular blood top-ups.
The world-first trial, underway in the UK, is studying whether red blood cells made in the laboratory last longer than blood cells made in the body.
Although the trial is only small, it represents a "huge stepping stone for manufacturing blood from stem cells," says University of Bristol cell biologist Ashley Toye, one of the researchers working on the study.
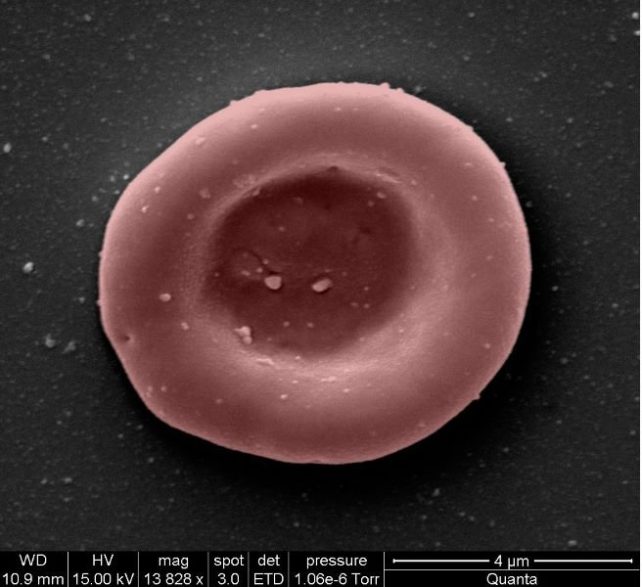
To generate the transfusions, the team of researchers isolated stem cells from donated blood and coaxed them into making more red blood cells, a process that takes around three weeks.
In the past, researchers showed they could transfuse lab-grown blood cells back into the same donor they were derived from. This time, they have infused the manufactured cells into another compatible person – a process known as allogeneic transfusion.
Only two people have so far received the lab-made red cells under close monitoring and "no untoward side effects" have been reported by the clinical team, according to a statement released last month.
At least another eight participants will receive two transfusions of 5 to 10 milliliters of blood, spaced at least four months apart. One transfusion will contain red blood cells provided by a donor; the other will have lab-grown red cells derived from stem cells from the same donor.
Once transfused into the bodies of healthy volunteers, the manufactured cells – which are labeled with a tracer dye – will be tracked as they whiz through the body's circulatory system, until they are worn out, gobbled up, and recycled.
The lab-grown blood cells are all freshly made from donated stem cells, whereas a typical blood donation contains a swirling mix of new and months-old blood cells, so the researchers are hopeful the manufactured cells will go the distance and last longer. Earlier animal studies suggest so.
The average lifespan of a human red blood cell is about 120 days. If the lab-grown cells can outlast donated blood cells, it could mean that in the future patients who regularly need blood may not need transfusions so often.
"If our trial, the first such in the world, is successful, it will mean that patients who currently require regular long-term blood transfusions will need fewer transfusions in future," says Cedric Ghevaert, a hematologist at the University of Cambridge and chief investigator of the trial.
Not only could the lab-grown cells reduce the frequency of blood transfusions for those in need, it could also help avoid complications linked to repeated infusions.
For instance, patients with blood disorders such as sickle cell disease often need regular blood transfusions, relying on the goodwill of blood donors and good fortune to find the right match. A person with sickle cell disease will receive blood transfusions to replace the misshapen red cells their body makes, to boost their oxygen levels.
Meanwhile, multiple transfusions can cause iron to accumulate in the body, a complication known as iron overload. Given long-lasting red cells, the risk of accumulated iron could be reduced.
Fewer transfusions could also lower the risk of repeat transfusion patients developing life-threatening immune reactions to specific donor blood groups. Too many transfusions of one blood type and the body might start producing antibodies against it.
One of the remaining questions is whether the process can be scaled up to produce greater volumes of blood needed in clinical care.
"At the moment, we are only infusing one to two teaspoons to our volunteers and normally, for a transfusion, you would be transfusing a hundred times that amount," explains trial investigator Rebecca Cardigan, a clinical scientist at the University of Cambridge.
More research is also needed to understand at what point blood-derived stem cells tire of making red cells, and need to be replenished with more donations.
"To go from here to a routine product for patients, there is obviously a lot more work that needs to be done that will take many years," Cardigan says in the video below, where you can see how the cells are made.
While they won't replace the need for blood donors, if the lab-grown cells prove to be safe and long-lasting, they could transform care for people with complex transfusion needs.
Manufacturing blood for those among us with ultra-rare blood types might also be a possibility.
"The need for normal blood donations to provide the vast majority of blood will remain," says Farrukh Shah, the medical director of transfusion for the UK National Health Service's Blood and Transplant unit.
"But the potential for this work to benefit hard-to-transfuse patients is very significant."