For a virus, spreading for a few months and reaching more than 3 million hosts is a long time span to evolve and change.
Some viruses - like influenza - mutate a lot, meaning that we need to update vaccines yearly to remain on top of the spread of seasonal flu. Meanwhile, the coronavirus that has caused the current COVID-19 pandemic has stayed relatively stable, and it seems to be mutating much more slowly than influenza.
This is great news for vaccine development and for the scientists who are closely studying the virus. But that doesn't mean it's not mutating at all.
Two new studies have recently been digging into the RNA genome of SARS-CoV-2, looking for mutations. One study, from Arizona State University, discovered a large base pair deletion in a virus sample taken from a patient in Tempe.
The second study, currently still a pre-print from the Los Alamos National Laboratory, tracked mutations throughout the outbreak, and hypothesised that one strain of the virus is more infectious than the original Wuhan strain.
The Arizona study generated three full-length SARS-CoV-2 genomes from a series of samples; they found that one of these genomes, which they've named AZ-ASU2923, had a large deletion - 81 base pairs - in a gene called ORF7a.
The ORF7a gene creates an accessory protein, which helps the virus infect, replicate and spread inside the human host. Specifically, the protein is thought to help the virus to evade our immune system and kill the cell once the replication process is complete.
"One of the reasons why this mutation is of interest is because it mirrors a large deletion that arose in the 2003 SARS outbreak," says one of the researchers, virologist Efrem Lim from Arizona State University.
Right now, we don't know how this mutation would change the coronavirus, and the researchers are investigating. Past research on similar genes and the fact it's only been found in a single individual, suggest that this deletion probably isn't great news for the virus.
"Similar deletions in SARS-CoV-2 genomes are emerging, notably in the ORF8 gene that may potentially reduce virus fitness," the team writes in their paper.
"Collectively, although global next generation sequencing efforts indicate that SARS-CoV-2 genomes are relatively stable, dynamic mutations can be selected in symptomatic individuals."
Meanwhile, the second study produced by a team at the Los Alamos National Laboratory has received significantly more media coverage, despite the fact it's currently in the pre-print stage, and therefore hasn't been peer-reviewed yet.
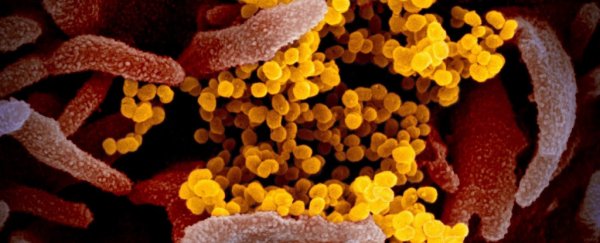
The Los Alamos team created an analysis pipeline to track the mutations seen in the coronavirus, particularly those mutations relating to the infamous spike protein on the surface of the virus.
The team found fourteen mutations relating to the spike, which are accumulating as the virus spreads. But one mutation in particular is worrying the researchers.
"The mutation spike D614G is of urgent concern; it began spreading in Europe in early February, and when introduced to new regions it rapidly becomes the dominant form," the team writes in the pre-print.
"There was, however, no significant correlation found between D614G status and hospitalisation status."
The mutation itself is much smaller than the Arizona one: it's a swap in a single base pair, although most of the cases also had two other single swaps in two other genes.
The team argues that because the D614G spike protein mutation has 'overtaken' the original Wuhan version (called D614) in a number of locations around the world, the D614G virus is more contagious, and felt an "urgent need for an early warning" in case the mutation affects the development of drugs and vaccines.
But not everyone agrees that the mutation has significantly changed the ability of the virus to spread.
"The great majority of sequenced isolates now descend from the European outbreak, which has spread more extensively than the Chinese one," Harvard University epidemiologist Bill Hanage told Gizmodo.
"That could be because it is more transmissible, but it could also be because the relatively late interventions allowed it to spread more."
Like everything else that has genetic material, viruses will slowly mutate as they produce more copies. SARS-CoV-2 is so far estimated to have a rate of less than 25 mutations per year, compared to influenza's 50.
Most mutations are neutral – they seemingly do nothing, while a few are deleterious, which will harm the virus and usually peter themselves out. Only a small percentage of all mutations are beneficial for the virus itself.
Although rare, beneficial mutations do happen in all sorts of organisms – antibiotic resistance in bacteria is one such example. But right now, we just don't know which type of mutation D614G is for the SARS-CoV-2 virus.
The good thing is that researchers are on the case, and we'll no doubt have more information soon. So, although an already dangerous and highly contagious virus mutating sounds incredibly nerve-wracking, don't stress too much. Viruses will mutate, and the coronavirus is no exception.
Scientists are on the case.
The Arizona paper has been published in the Journal of Virology, and the Los Alamos paper is available on pre-print server bioRxiv.
Editor's note (7 May 2020): This article has been updated to clarify that SARS-CoV-2 is an RNA virus, and doesn't contain DNA. We apologise for the error.