With age, our bodies get to enjoy some weird and wonderful things. Our brains go a little foggy, we make more noises when we stand up, and new research has found we might even end up with tiny bone-like particles running around the bloodstream.
That kind of stuff coursing through your blood vessels doesn't sound good - obviously - but this finding might take us closer to understanding some of the issues that may strike our cardiovascular system with age.
We've long known that sometimes tissue within the human body can start to resemble bone. This is due to a process called calcification – the accumulation of calcium salts in said tissue. Such accumulation can present as gallstones or kidney stones, become bone spurs, or even end up in other parts of the body.
Sometimes, this mineral build-up can happen in blood vessels, leading to the unsurprisingly named vascular calcification. This process is associated with ageing, but can also be linked to diabetes, hypertension, or kidney disease.
Despite knowing that vascular calcification happens, researchers still don't have a complete picture of the processes inside our blood that lead to minerals accumulating in the walls of our blood vessels.
In this latest study, researchers led by University of Texas kinesiology professor Rhonda Prisby now report the presence of strange bone-like particles - and they could have something to do with vascular disease.
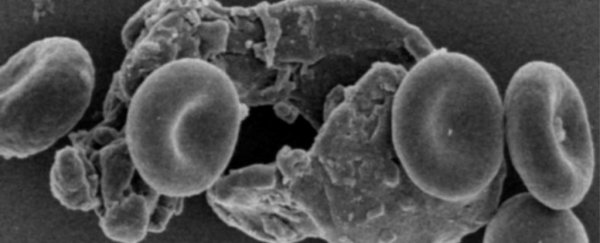
"The major finding of this investigation is the discovery of bone-like particles in the peripheral circulation of humans and rats," the team writes in their paper.
In a previous study authored by Prisby, she characterised severe calcification in the blood vessels that are found in bone marrow, indicating that both in rat samples and human patients these vessels looked as if they'd turned to bone, or ossified.
The investigation also indicated the presence of bone-like particles in those ossified blood vessels. So in this study, the researchers explored further to see if these particles might move from bone marrow into peripheral circulation.
"Presumably, ossified particles originate during the processes of bone marrow blood vessel ossification and are capable of entering into the peripheral circulation," the team writes.
"Thus, in addition to examining ossified bone marrow blood vessels via ultra-high microscopy, we sought to confirm, characterise and quantify the presence of ossified particles in peripheral whole blood samples from humans and rats."
Although the researchers used only a small number of human samples - including bone marrow vessels in a tibia coming from an amputated leg, and blood samples from 12 volunteers - the results are rather interesting, and a little concerning.
"While the majority of the ossified particles were small in diameter (15 μm) to block small blood vessels throughout the vascular tree," the researchers explain in their study.
Although the number of ossified particles didn't appear to increase with the age of the patient, the size of them did. The six younger patients had particles ranging in size from 1-29 μm, while the six older patients' particles ranged from 1-66 μm.
The team also investigated the size of these particles in rats, but found that there were no significant changes by age, although there was a limitation in being able to discern bone-like particles from the tiny blood cells called platelets.
"Future investigations will require the elimination of platelets from the whole blood sample in order to decipher any age-related increases in the number of [bone-like particles]," the team notes, adding the importance of larger sample sizes to further investigate this phenomenon.
The most important aspect of these particles might well be their shape - a potential clue to how their circulation in the blood could contribute to the development of cardiovascular problems.
"Some of the ossified particles have sharp tips and edges that could damage the lining of blood vessels," says Prisby.
"This damage could initiate events leading to atherosclerosis (build-up of plaque), which can restrict blood flow over time."
The research has been published in Microcirculation.