Bone marrow cells in the skull have a distinct response to disease, and scientists say this means the skull could be a useful way to watch and potentially treat inflammation in the brain.
A research team from Germany and the UK investigating this reaction proposes their findings could serve as a non-invasive skull imaging technique.
"This opens up a myriad of possibilities for diagnosing and treating brain diseases and has the potential to revolutionize our understanding of neurological diseases," says neuroscientist Ali Ertürk from Munich University in Germany.
"This breakthrough could lead to more effective monitoring of conditions such as Alzheimer's and stroke, and potentially even aid in preventing the onset of these diseases by enabling early detection."
Neuroinflammation plays a significant role in many disorders of the brain and nervous system, activating immune cells and releasing inflammatory molecules that help protect and heal our tissues. Yet it can come at a cost, risking damage and compromising healing. What's more, the skull and other membranes protect the brain, making accessing it for treatment of errant inflammation challenging.
Scientists have recently discovered pathways from the bone marrow of the skull through the brain's outermost surface of the protective membranes, the meninges, permitting immune cell movement and challenging the notion that the skull and the brain have no direct interchange.
It's well known that immune cells can enter the brain after problems such as strokes cause the blood-brain barrier to weaken, but how immune cells enter the brain layers via the skull and how often they access them this way compared to other routes are unclear.
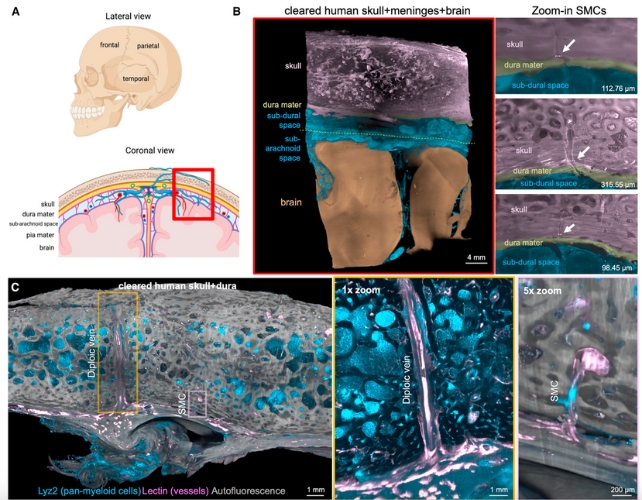
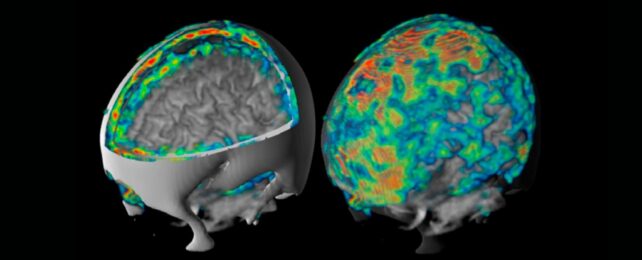
In experiments to visualize human brain, meninges, and skull samples, the team used tissue clearing in combination with 3-D imaging.
Tissue clearing is the process of treating biological tissues to make them transparent. In this context, the process allowed light to pass through for microscopic examination of brain tissue and the skull.
The researchers observed cellular architecture of the skull-meninges connections (SMCs) that extend closer to the brain's surface than was previously believed, often penetrating that outermost and toughest meninges membrane, the dura mater.
"These findings carry profound implications, suggesting a far more complex connection between the skull and the brain than previously believed" says Ilgin Kolabas, a neuroimmunologist from Munich University.

Kolabas and colleagues also studied cells from six different bones, the dura mater, and the brain, finding different bones have different molecular profiles, with unique immune cells detected in the skull.
Protein analysis of human postmortem skull, spine, and pelvic bone samples once again uncovered the skull's unique molecular profile. The calvaria, which forms part of the top of the skull, had the most differentially expressed genes and cellular receptors, mostly related to migration and inflammation.
The team also found both human and mouse skulls contain specialized neutrophil cells, a type of white blood cell that plays a crucial role in the body's immune defense.
Using a form of functional imaging called positron emission tomography (PET), the team detected changes in signals in the skull that mirror those from the underlying brain in human patients with Alzheimer's disease and stroke. They also detected increases in disease-specific translocator protein (TPSO) signals in various parts of the skull in many neurological diseases.
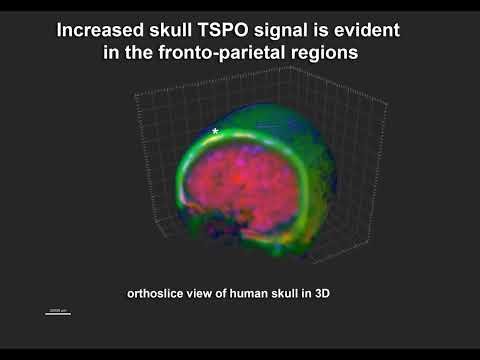
The scientists think their new discoveries about the skull's immune response suggest it's possibile to detect brain inflammation with little more than a scan of a patient's skull.
"This could potentially be done using portable and wearable devices, offering a more accessible and practical way to monitor brain health," Ertürk explains.
Alzheimer's disease, stroke, and multiple sclerosis are just a few examples of neurological disorders that affect millions of people around the world.
"Our detailed demonstration of skull inflammation in diverse diseases in humans suggests that it can be used for diagnosing or monitoring diseases in the future," the team concludes, "but detailed clinical studies are needed to explore its clinical utility."
The study has been published in the journal Cell.
