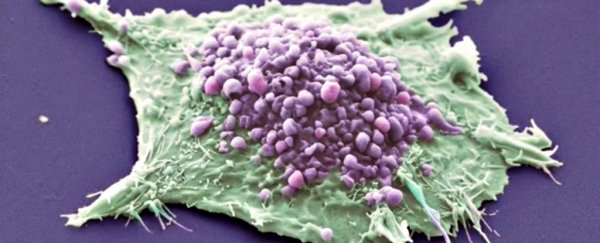
Scientists just took a big, "very positive" step towards developing what could be the first 'universal cancer vaccine'.
The results from early trials in humans, along with research in mice, have just been published, and they suggest that the new technique could be used to activate patients' immune systems against any type of tumour, no matter where it is in the body.
Unlike the vaccines we're familiar with, this potential vaccine would be given to patients who already have cancer, rather than those at risk of getting it. It basically works by shooting tiny 'darts' containing pieces of RNA extracted from the patient's cancer cells at the body's own immune system, convincing them to launch an all-out attack on any tumours they come across.
By just changing the RNA inside those darts, the team can, in theory, mobilise the immune system against any kind of cancer. "[Such] vaccines are fast and inexpensive to produce, and virtually any tumour antigen can be encoded by RNA," the team, led by researchers at Johannes Gutenberg University of Mainz in Germany, reports in Nature.
"Thus, the nanoparticulate RNA immunotherapy approach introduced here may be regarded as a universally applicable novel vaccine class for cancer immunotherapy."
Immunotherapy, which involves using the patient's own immune system to attack cancer, isn't in itself new - researchers are already using it against different cancer types with great results.
But until now, researchers have mostly done this by genetically engineering special, cancer-targeting immune cells in the lab, and then injecting them back into a patient - which is a time-consuming and expensive process.
The difference with this technique is that the vaccine is made in the lab, and it introduces the cancer DNA into the immune cells within the body, which is a lot less invasive. It also means that the vaccine can be tweaked to hunt a range of cancer types.
So why isn't the immune system naturally taking out these cancer types?
"One reason is that cancer cells are similar in many ways to normal cells and the immune system avoids attacking the self," explain Dutch immunologists Jolanda de Vries and Figdor in a commentary accompanying the Nature paper.
That means that when you develop a vaccine, you need to use an antigen - a foreign molecule that works like a 'mugshot' for the immune system - that's not expressed in normal cells, too.
"Only relatively modest immune responses occur with vaccines containing antigens that are also expressed on healthy tissue," write de Vries and Carl Figdor. "Strong immune responses can be expected only when cancer cells express antigens that are not usually expressed in normal adult cells."
It's this kind of cancer-specific antigen that the new vaccine is designed to deliver to the immune system. It works by coating the cancer RNA in a simple, fatty acid membrane, and giving it a slightly negative charge.
This means that once the vaccine is injected into a patient, it's drawn via electric charge towards dendritic immune cells in the spleen, lymph nodes, and bone marrow.
These dendritic cells then 'show' the cancer RNA to the body's T cells and, to anthropomorphise the situation, pretty much tell them, "Hey, this is the guy we're after, go get him." The goal is that the T cells will then go out and mass murder all the cancer cells in the body.
And this is what early research by the German team has demonstrated in mice. Once injected with the vaccine, the immune system was able to fight "aggressively growing" tumours, the research found.
Of course, many results in mice don't translate to humans, so we can't get too excited just yet.
The team has also now trialled a version of the vaccine in three patients with melanoma. The point of the trial was only to test whether the vaccine was safe to use in humans, not whether it was effective, and so far, the results are promising. The side effects were limited to flu-like symptoms, which is better than most chemotherapy treatments.
The team is now waiting 12 months for follow-up results from this safety trial, and if all goes well, will start a larger clinical trial after that to see if the vaccine really works.
"By combining laboratory-based studies with results from an early-phase clinical trial, this research shows that a new type of treatment vaccine could be used to treat patients with melanoma by boosting the effects of their immune systems," Aine McCarthy, the senior science information officer at Cancer Research UK, told The Telegraph.
"Because the vaccine was only tested in three patients, larger clinical trials are needed to confirm it works and is safe, while more research will determine if it could be used to treat other types of cancer."
Although it's still very early days, we have another reason to feel hopeful about the future of cancer treatment. And that's always a good thing.