Researchers have found a new target for a potential HIV vaccine, and they already have evidence in the lab that it can stop the virus from infecting cells.
The new target is part of the HIV envelope called the 'fusion peptide', and its structure is simpler than the sites that past HIV vaccine attempts have focussed on. This offers hope that, this time, we might have more luck getting the body to recognise and shut down the virus before it's too late.
Vaccines work by exposing the immune system to a harmless part of a virus, and priming it to attack it next time it sees it - hopefully shutting down infection before it happens. But although we've seen more than 100 HIV vaccine candidates being trialled over the past 30 years, so far, none of them have reliably been shown to offer humans long-term protection.
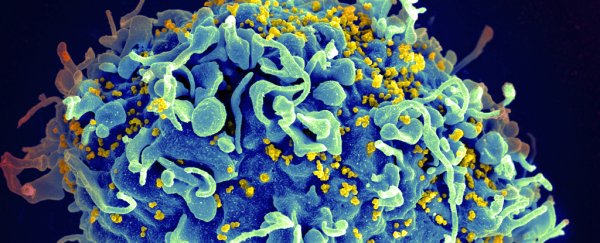
That's because HIV is a tricky beast - it infects white blood cells called T-cells and then hijacks our immune system and uses it against us. So once the virus has infected a T-cell, it's pretty much invisible to the immune system.
As we reported last year, the best chance we have to prevent infection "is to trigger antibodies against the HIV surface proteins before that happens - something that's been equally difficult considering the fact that the retrovirus can regularly change its viral envelope to hide particular surface proteins".
So it's no surprise that scientists have struggled. In fact, for the past couple of years, many teams have focussed on developing long-acting antibody injections for protection, instead of trying to make vaccines.
What's new about this vaccine target is the fact that it was identified by studying the blood of a rare, unnamed HIV-positive patient, who makes antibodies against parts of the virus that aren't usually targeted - and is therefore better at fighting off symptoms.
When a team from the US National Institute for Allergy and Infectious Diseases (NIAID) analysed his blood, they found that his body was making a never-before-seen type of neutralising antibody, which they called the ever-so-easy-to-remember N123-VRC34.01, or VRC34.01 for short.
Long name aside, what's special about that neutralising antibody is that it attacks the fusion peptide - a string of eight amino acids that help the virus fuse with the cell.
That's a big deal, because " viruses often try to mask such key components of their cell entry machinery from antibody attack", the researchers write in Science.
But not only that, when they extracted this antibody and tested it in the lab, they found it actually stops HIV from infecting the cell altogether.
To figure out what was going on, they crystallised the antibody while it was attached to the virus - freezing it in time to see what was happening.
"This allowed them to characterise in atomic-level detail how VRC34.01 attaches to HIV and revealed that the antibody stops the virus from infecting a cell by binding to a key cell-surface molecule," a NIAID press release explains.
To get an idea of whether this might work in other people, they looked at the blood of 24 other HIV-positive patients and found that it wasn't actually uncommon for the immune system to try to attack the fusion peptide - 10 of those tested had antibodies targeting a similar site to VRC34.01.
But these other antibodies weren't as powerful at shutting the infection down, which suggests that if researchers can figure out a way to stimulate the body into creating VRC34.01 specifically, prior to being exposed to the virus, they might be able to achieve long-term protection against infection.
That's exciting, but the team still has a long way to go before they can turn this research into a vaccine candidate.
They're now figuring out how they can trigger the production of the new antibody en masse, and whatever they come up with will need to be tested in the lab and animal models before we get anywhere near lengthy human trials. As with all science, there's a lot that can go wrong in the meantime. In other words, all we have right now is a target - we still need to build a gun from scratch.
But any research that takes us closer to some kind of long-term protection against HIV - which still infects around 2 million people each year in the US alone - is worth pursuing.