Long before Alzheimer's disease is diagnosed, once-trusty proteins start to knot together in the brain in a process that may be hastened by poor sleep.
Now, scientists have uncovered a possible mechanism linking disruptions in circadian rhythms and the build-up of proteins associated with Alzheimer's disease, by studying the rhythmic operation of immune cells and finding the molecular 'timers' that control them.
Circadian rhythms are the daily rhythms of bodily functions which are tied to our natural body clock, respond to light exposure, and govern our sleep-wake cycles.
Poor sleep habits can throw circadian rhythms out of whack (aging and stress also don't help) and patchy sleep would mean less time for immune cells to cleanse the brain of waste products that build up throughout the day.
Sleep disturbances starting years before any symptoms emerge have been linked to a greater risk of developing Alzheimer's disease, the most common form of dementia, and more severe symptoms.
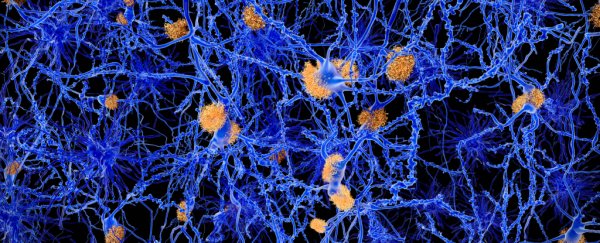
It's long been thought that over time, clumps of misfolded proteins – including one called amyloid-beta – accumulate in the brain to cause Alzheimer's disease, which is a neurological condition marked by memory loss and slow cognitive decline.
Daily fluctuations in levels of amyloid-beta have been noted in the cerebrospinal fluid of healthy adults, but these oscillations appear to be disrupted with age, the largest risk factor for Alzheimer's disease.
However, making the direct connection between circadian rhythms and the activity of immune cells tasked with cleaning up amyloid proteins has eluded scientists thus far.
In this new study, researchers led by biological scientist Jennifer Hurley of Rensselaer Polytechnic Institute studied immune cells called macrophages, which are known to migrate into the brain in late-stage Alzheimer's disease. Macrophages are scavengers that gobble up waste products, faulty proteins, and defunct cells to prevent toxic damage.
In lab-grown cell cultures observed under a microscope, these immune cells – derived from genetically modified mice with altered circadian clocks – went about cleaning up fluorescently-tagged amyloid-beta proteins on a daily cycle. As levels of cell-surface proteins called heparans went up, the clearance of amyloid-beta proteins slowed.
But the immune cells promptly lost their rhythm when their circadian clock was disturbed, suggesting cell-surface heparans, and the protein-eating immune cells they regulate, fall under circadian control.
"These data highlight that circadian regulation in immune cells may play a role in the intricate relationship between the circadian clock and Alzheimer's disease," the team writes in their paper.
Past research has found that just one night of bad sleep causes an increase in amyloid-beta proteins, and a week of sleepless nights leads to a build-up of another protein called tau, too. Chronic sleep problems could therefore spell trouble.
Whether circadian clock disruptions are a causative factor or physiological consequence of Alzheimer's disease is still unclear, though.
Keep in mind this study, which aimed to dissect possible mechanisms linking circadian clock disruptions and Alzheimer's disease proteins, used immune cells sampled from the bone marrow of genetically modified mice as a proxy for what happens in humans.
"With regard to the nature of the circadian disruption that occurs in AD, there is much still to be understood," behavioral neuroscientist Andrew Coogan of the University of Ireland and colleagues wrote in a 2013 review, which still rings true.
It's worth remembering, too, that amyloid proteins are not the whole story in Alzheimer's disease. Tangles of tau proteins are the other prime suspects which have come into focus in the wake of disappointing clinical trials and mounting evidence against amyloid-beta (Aβ) as the main culprit of disease.
"Though targeting Aβ as a therapeutic strategy has met limited success, Aβ accumulation is still regarded as a crucial step in AD pathogenesis," Hurley and colleagues write.
However, other recent research suggests amyloid proteins are actually latecomers to the disease rather than an early trigger, and poor sleep isn't the only risk factor for Alzheimer's disease.
That said, pinpointing a possible mechanism that goes some way to explaining how disruptions in circadian rhythms may perturb the clearance of amyloid proteins in the brain is a good step.
In a roundabout way, this work supports other lines of research looking at so-called chronotherapies, which are interventions that aim to improve people's sleep cycles.
Understanding the circadian timing of immune cells may also have implications for other disorders that like Alzheimer's disease are linked to inflammation, including depression.
"Understanding how our circadian rhythms can regulate cell-surface heparan levels to control the build-up of amyloid-beta may lead to the development of chronotherapeutics that alleviate the symptoms of Alzheimer's disease as well as other inflammatory diseases," Hurley says.
The study was published in PLOS Genetics.