Despite all our advances in cancer research, our best strategy of fighting the disease is still brute force, with only a fraction of the drugs administered actually reaching the tumour cells, and most being absorbed into healthy tissue. When cancer spreads, the likelihood of medication reaching it gets even lower, which is why secondary, or metastatic, tumours can be so deadly.
But now, researchers have used cancer's own tricks against it, by developing dissolvable nanoparticles that target the heart of metastatic tumours directly. And they've already seen unprecedented success in mouse studies, with 40-50 percent of the animals being "functionally cured", and tumour-free after eight months - the equivalent of about 24 years for a human patient. The team is so excited by these results, they hope to fast-track the research and begin human trails in 2017.
"I would never want to overpromise to the thousands of cancer patients looking for a cure, but the data is astounding," said one of the researchers, Mauro Ferrari, from the Houston Methodist Research Institute. "We're talking about changing the landscape of curing metastatic disease, so it's no longer a death sentence."
Right now, most fatal cases of cancer are metastatic, which is where cancer cells spread from a primary location to form secondary tumours, usually in the lungs and liver. Although we are making leaps and bounds in treating primary cancers, currently there is no cure and limited treatment for those with metastatic tumours.
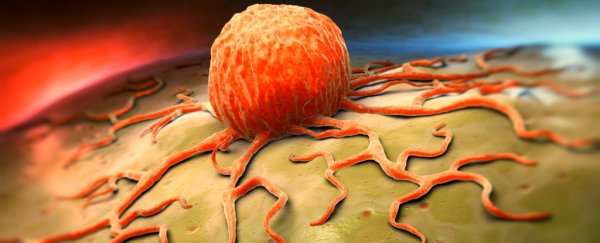
So how does this new treatment work? The key is something called an injectable nanoparticle generator (iNPG), which is the right size and shape to be able to move through the regular blood vessels unimpeded.
But cancer triggers the body to create new blood vessels, as they need more oxygen than non-cancerous tissue. When the nanoballs reach these cancer-formed blood vessels - which the iNPG can identify because they're malformed and leaky - the device is able to enter the tumours and break them down over two to four weeks, releasing polymer strands laced with a potent cancer drug called doxorubicin, or dox.
Dox has been used in cancer treatment for years, because it jams the DNA replication mechanism and prevents tumour cells from dividing. But, as with many existing cancer treatments, that means normal cells also suffer, and it can kill heart muscle cells, and potentially cause heart failure.
Usually, dox can't get near the nucleus of a cancer cell, which is where it needs to do damage, because the membrane of tumour cells filter it out. But by releasing dox inside polymer strands, which fold up into tiny nanoballs, researchers have found a way for it to be welcomed in by cancer cells, allowing it to get right to the heart of the tumours.
"We invented a method that actually makes the nanoparticles inside the cancer and releases the drug particles at the site of the cellular nucleus," said Ferrari. "With this injectable nanoparticle generator, we were able to do what standard chemotherapy drugs, vaccines, radiation, and other nanoparticles have all failed to do."
As Robert Service from Science explains, the team isn't quite sure why the tumour cells ferry the dox-containing nanoparticles towards the cell nucleus, but it's exactly what they wanted to happen:
"Not only is the region around the nucleus devoid of dox-removing pumps, but it typically has a more acidic environment than near the cell membrane. And Ferrari's team used this to their advantage as well. They designed the chemical links between dox molecules and the polymer to dissolve under acidic conditions. This releases the dox at the site where its cell killing potency is highest."
We've reported on nanoparticles fighting cancer before, but these results in mice are a first, and those in the field are showing cautious optimism. Although the iNPG system is only been shown to target metastatic breast cancers at this stage, it has the potential to be used to treat cancer that has metastasised to the lungs and liver.
"If this research bears out in humans and we see even a fraction of this survival time, we are still talking about dramatically extending life for many years," said Ferrari. "That's essentially providing a cure in a patient population that is now being told there is none."
The study has been published in Nature Biotechnology.